CONFERENCE COVERAGE SERIES
Society for Neuroscience Annual Meeting 2006
Atlanta, GA, U.S.A.
14 – 18 October 2006
CONFERENCE COVERAGE SERIES
Atlanta, GA, U.S.A.
14 – 18 October 2006
On Friday, October 13, the day before the kick-off of the Society for Neuroscience meeting in Atlanta, Lary Walker of Emory University, Atlanta, Georgia, and Richard Kostrzewa of East Tennessee State University in Johnson City, hosted a satellite symposium at the Yerkes National Primate Research Center on the Emory campus. Sponsored by the Neurotoxicity Society, the symposium brought together a distinguished slate of speakers who considered the central, yet unsolved question of Alzheimer disease, and neurodegeneration in general—how exactly do neurons die? Two talks highlighted novel players in AD. One, by Gilles Guillemin from the University of New South Wales, Sydney, Australia, focused on the production of the excitotoxic tryptophan metabolite quinolinic acid by activated microglia and macrophages. The other came from Efrat Levy, Nathan Kline Institute in Orangeburg, New York, on the neuroprotective actions of the protease inhibitor cystatin C. Bill Klein, Northwestern University, Chicago, talked about the hottest topic in Aβ toxicity—oligomers. In addition, Todd Golde, Mayo Clinic, Jacksonville, Florida, presented his work on the use of adeno-associated viral vectors. He has used these to generate quick in-vivo animal models of neuron death in order to investigate the proteins and pathways that precipitate neurodegeneration.
There are over a hundred naturally occurring AAV variants showing a range of tissue tropism suitable for gene delivery, but most of them have not been studied in the CNS, Golde said. Work done largely by Ronald Klein at Louisiana State University Health Sciences Center in Shreveport showed that injecting AAV8- or AAV1-encoding green fluorescent protein into the rat hippocampus could drive long-term, high-level expression of GFP mostly in neurons (Klein et al., 2005). Comparison of different AAV serotypes showed that some gave better dispersal through the brain tissue, while others drove higher expression. When Golde and colleagues looked in the mouse, the serotypes behaved differently than in rats, suggesting that a trial-and-error approach to evaluate multiple serotypes is necessary to optimize gene delivery in different species.
Though AAV-mediated delivery of genes can save time and money compared to traditional transgenic construction, the resulting animals are far more than a poor person’s transgenics. Viral delivery makes it possible to look quickly at the effects of nearly any protein solely in the brain and in different species, including mice, rats, or even guinea pigs. Golde showed that AAV can be used to make a rat model of β amyloid expression by introducing the Aβ1-40 or Aβ1-42 peptide fused to the Bri protein, which has a furin cleavage site (see ARF related news story). In collaboration with Trish Lawlor and Matt During at the University of Auckland, New Zealand, and Ross Bland at Neurologix Inc., New York, Golde found that the Aβ42 fusion causes plaque formation and behavioral impairments in animals. The approach can even be used in guinea pigs, an attractive model for several reasons: guinea pig Aβ sequence is identical to the human peptide; the animals handle cholesterol and lipoproteins more like humans; and they have a more active inflammatory response compared to mice or rats.
In mice, Golde described the production of “somatic brain transgenics,” where recombinant AAV virions were injected freehand into the ventricles of newborn cryo anesthetized mouse pups. This procedure was originally described by John Wolfe and colleagues (Passini and Wolfe, 2001) but has not been widely applied. The procedure takes 15 minutes per litter, and with AAV1, yields lifelong transduction of the cortex and hippocampus. With the AAV9 serotype, they saw almost all neurons in the brain transfected using a GFP reporter.
Golde reported that in one study, using the vectors to introduce single-chain antibodies to Aβ40, Aβ42, or a pan-specific antibody, he found all the proteins attenuated plaque deposition in CRND8 mice as effectively as the passive immunization they previously reported with antibodies of the same specificity (see ARF related news story). But the AAV study was cheaper and faster, being completed in 5 months at a fraction of the cost of a breeding study. The second study, which was largely carried out by Andrew Nyborg in Golde’s lab, involved expressing a mutant non-cleavable form of pro-NGF. Previously, other researchers had shown that pro-NGF induces neuron death via the SorLa family receptor sortilin and the p75NGF receptor (Nykjaer et al., 2004). Introduction of a non-cleavable pro-NGF caused build-up of the pro-peptide over the first weeks of life, and early death of the mice, which was not seen with either sortilin overexpression or introduction of wild-type pro-NGF. The brain tissue had increased astrocytosis, microgliosis, tau phosphorylation, and apoptotic cells. The entire study took 3 months, Golde said. Compared to transgenics, the method is cheap, fast, reproducible, flexible (vectors can accommodate shRNAs, for example), and great for proof-of-concept studies. Right now, the technique works best on young mice, and Golde says they want to get to where they can transduce the whole brain in adults as well.
Moving on to other neurotoxic pathways, Guillemin, a neuroimmunologist working with Bruce Brew and Karen Cullen in Sydney, gave a primer on tryptophan oxidation and outlined some data connecting this inflammation-related pathway to Alzheimer disease. The bottom line is that the induced catabolism of tryptophan to form the excitotoxin quinolinic acid may be one reason why inflammation is dangerous to neurons.
The metabolism of the essential amino acid tryptophan is initiated during immune responses by the cytokine-induced expression of the enzyme indoleamine 2,3-dioxygenase (IDO). This enzyme catalyzes the rate-limiting first step in the catabolism of Trp down the kynurenine pathway. The resulting depletion of cellular tryptophan inhibits the replication of intracellular pathogens, and also plays a role in immune tolerance by inhibiting T cell activation. One downstream product of the pathway is quinolinic acid (QA), an excitotoxin that binds to NMDA receptors. QA also increases glutamate release by neurons, blocks glutamate uptake by astrocytes, and can induce apoptosis in astrocytes. IDO protein and QA are both increased in AD brain (Guillemin et al., 2005). In vitro treatment with Aβ42, but not 40, induced IDO expression in macrophages, and to a lesser extent human fetal microglia. This suggests that macrophages and microglia around plaques might be producing quinolinic acid, and Guillemin showed that in moderate stages of AD, microdissected amyloid plaques which were surrounded by activated macrophages and microglia contained a lot of quinolinic acid, but in later disease, where inflammation was less apparent, there was less.
QA is not produced by neurons, but immunostaining showed it to be present in neurons from AD brains. How does it get there? To answer this question, the researchers applied QA to brain tissue, and saw uptake into vacuoles in neurons. They also presented data that QA induces γ-secretase activity, tau phosphorylation and apoptosis in cultured neurons. QA also activates astroglia, which could amplify IDO expression by making more cytokines. These results suggest that QA could play a role in inflammation-mediated neurodegeneration. Specific kynurenine pathway inhibitors are now in clinical trials for stroke. If the QA hypothesis is correct, these might be expected to be of some use in AD.
From neurotoxicity to neuroprotection. Efrat Levy, Nathan Kline Institute, Orangeburg, New York, showed new data supporting the role of the endogenous protease inhibitor cystatin C as a neuroprotective agent in AD. By way of background, cystatin C inhibits the cathepsin cysteine proteases, which play a role in many diseases. In AD, cathepsin B in particular has been implicated as a β-secretase and more recently, as an Aβ-degrading enzyme (see ARF related news story).
Cystatin C first came to attention when it was recognized that a mutated form of the protein causes cerebral amyloid angiopathy. But another genetic variant, the CST3 polymorphism has been associated with late-onset AD, and works in conjunction with ApoE4 to increase risk for the disease. The polymorphism is associated with decreased secretion of the protease inhibitor, and decreased levels of it in the CSF.
Previously, Levy showed that cystatin C binds to soluble Aβ and to the Aβ region of APP, and exerts an anti-aggregation activity. It is found in plaques, perhaps carried there by soluble Aβ. Consistent with an anti-plaque activity, Levy’s new results showed that crossing a cystatin C transgenic mouse with the Tg2576 or APP23 mouse caused a reduction in plaque load at 18 or 12 months, respectively. The cystatin C transgenic mice displayed no changes in Aβ production, but there was a reduction in fibrillar Aβ in the crossed mice.
Cystatin C expression is known to increase in response to injury—but is it neuroprotective? Adding cystatin C (0.2-0.4 μM) directly to N2a cells in culture protected them from serum deprivation. The same conditions also protected cells from toxicity of preformed Aβ fibrils. The protection was not due to dissolution of the fibrils, since incubation of preformed Aβ fibrils with cystatin C did not dissolve the fibrils, but did prevent their toxicity. Finally, Levy showed that cystatin C also protected the cells against toxicity of Aβ oligomers. Recent data on cathepsin B knockout mice (see ARF related news story) suggested that cathepsin B protects from amyloid toxicity by degrading fibrillar Aβ, but this new data shows that cathepsin B inhibitor is protective. How can these results be reconciled? Levy says the investigators are currently studying how cystatin C levels affect cathepsin B and D activity in the cells and in animals. Levy thinks the neuroprotective effects of cystatin C may not involve cathepsins directly, but may instead involve the induction of protective autophagy in response to the stress of serum deprivation.
Bill Klein, Northwestern University, Chicago, presented some new data on the action of Aβ oligomers, or ADDLs, on neurons. He showed that memantine, the NMDA receptor antagonist and memory enhancer, blocks the ability of Aβ oligomers to increase reactive oxygen species in neurons. Antibodies to the NMDA receptor N-terminus, but not its C-terminus, had the same effect. The results focus attention squarely on the NMDA receptor as a mediator of the toxicity of Aβ oligomers, but the identity of any protein receptor for these Aβ assemblies remains unknown. Klein said they have isolated a large receptor complex, but have not identified the ADDL binding site.—Pat McCaffrey.
The yin and yang of transforming growth factor β (TGF-β) is nowhere more apparent than in Alzheimer disease. It’s been known for over a decade that expression of the cytokine is increased in AD brain (Flanders et al., 1995). Tony Wyss-Coray and colleagues showed that TGF-β overproduction by astrocytes is neuroprotective, and that TGF-β1 knockouts display increased neuronal death (see ARF related news story). That group also showed that TGF-β promotes clearance of Aβ by microglia and protects mice from Aβ deposition (Wyss-Coray et al., 2001). Conversely, the same researchers showed that high TGF-β levels in mice cause cerebrovascular amyloid angiopathy (Buckwalter et al., 2002), and Denis Vivien and colleagues tied high TGF-β to elevated APP expression and Aβ production (see ARF related news story). One difficulty in sorting out the risk/benefit ratio for TGF-β is that many cells in the nervous system and beyond respond to the cytokine, making it hard to know which players mediate various effects.
Two new studies, one just published and one presented for the first time at the Society for Neuroscience annual meeting in Atlanta, Georgia, last month, attempt to get at this question, not by knocking out the production of TGF-β, but instead by blocking its signaling in selected groups of target cells. Both take a similar approach of engineering transgenic mice to carry a dominant negative form of the TGF-β type II receptor. But in one study, the dominant negative was expressed in neurons, while in the other it was in peripheral macrophages, and that change in location turns out to make a world of difference.
In the first case, work from Tony Wyss-Coray and colleagues at Stanford University Medical School, California, shows that impeding neuronal TGF-β signaling promotes neurodegeneration and can exacerbate amyloid pathology in AD mice. That study, published in the November issue of the Journal of Clinical Investigation, contrasts with unpublished data presented at the SfN meeting that showed getting rid of TGF-β signaling in peripheral macrophages has an anti-amyloid effect. There, Terrence Town of Yale Medical School, New Haven, Connecticut, showed that damping down TGF-β action seems to unleash the Aβ-gobbling tendencies of macrophages. When taken together, the results from both groups suggest that boosting TGF-β centrally, or inhibiting it peripherally, might both be viable approaches to reducing amyloid deposition.
The study of neuronal TGF-β starts with first author Ina Tesseur and colleagues showing that the levels of the high-affinity TGF-β type II receptor subunit protein are decreased to about half of normal levels in brain tissue from people with AD. The decline is apparent early—in AD patients with mild dementia. It appears specific for AD, and was not observed in postmortem brain from patients with other neurodegenerative disorders, including Parkinson disease or progressive frontotemporal dementia. Immunostaining of brain sections revealed the receptor was mainly present on neurons, with far fewer in astrocytes. These results, along with the same group’s previous observations that TGF-β is increased in AD brain, suggest that something is amiss with this cytokine pathway in this disease.
To find the possible consequences of decreased TGF-β signaling in neurons, the researchers produced transgenic mice that expressed the TGF-β receptor type II with a deletion of the cytoplasmic serine/threonine kinase domain. This protein acts as a dominant negative inhibitor of endogenous receptor signaling, and its expression was restricted to cortical and hippocampal neurons with the neuron-specific prion promoter and tetracycline-sensitive expression.
Consistent with TGF-β’s neurotrophic actions, cultured neurons from the transgenic mice showed increased cell death, and the animals demonstrated age-dependent neuron loss in vivo, as indicated by significant decreases in MAP2, synaptophysin, and NeuN immunoreactivity in very old mice (34 months of age) compared to control animals. GFAP was elevated, indicating ongoing astrocytosis.
When they looked for AD pathology in the transgenics, the researchers found a trend toward elevation of Aβ, but the increase did not reach significance, and no amyloid deposits were observed. When they crossed the dominant negative mice with J20 mice, which express human APP with the Swedish and Indiana mutations, however, they did get enhanced Aβ accumulation. Amyloid deposition and thioflavin S deposits were increased about twofold in old crossed mice (20 months), but not in younger ones (14 months or younger). A decrease in MAP2 immunoreactivity indicated neuronal loss as well, which was not seen in TGF-βRII transgenics at the same age.
While the researchers found no evidence in the mice for enhanced APP expression or processing, or decreased Aβ degradation, studies in cultured cells pointed to an increase in Aβ production when TGF-β signaling decreased. In rat neuroblastoma cells expressing human APP, they saw an increase in Aβ secretion in response to either the dominant negative receptor, or a kinase inhibitor of TGF-β signaling. Inhibiting TGF-β action resulted in beading and retraction of neurites and rounding and detachment of cells, independent of whether the cells also expressed APP or not. These results suggest that TGF-β is necessary to maintain the health and integrity of cells, and that its reduction may promote APP processing and Aβ production.
“Collectively, these studies suggest that defects in TGF-β signaling may contribute to AD pathogenesis by promoting neurodegeneration and initiating a feedback loop in which the degenerating cell produces more Aβ, thereby enhancing amyloid deposition,” write Pritam Das and Todd Golde, Mayo Clinic, Jacksonville, Florida, in an accompanying piece. More work will be needed to find out why the TGF-β receptor is downregulated in AD brain (perhaps in response to upregulation of TGF-β itself?), how this alters Aβ production, and whether changes in processing explain the increased amyloid deposition observed in crossed mice.
Separate from its neurotrophic actions, TGF-β plays an important role in the immune response, and Town’s SfN talk focused on the interplay between the worlds of the CNS and peripheral innate immune system. Town, a researcher in Richard Flavell’s lab at Yale, hooked up the TGF-βRII dominant negative to the CD11c promoter to create mice lacking TGF-β signaling in cells of the innate immune system, including macrophages and dendritic cells (but not microglia). When he crossed these mice with Tg2576 AD mice, he saw their cortical and hippocampal plaque load and Aβ peptide content reduced by 60-80 percent at 18 months. The mice also showed a dramatic 60-90 percent reduction in cerebral vascular amyloid, and reduced astrogliosis. These changes were associated with behavioral differences, as the crossed mice showed less hyperactivity in a novel environment and in the Y maze compared to the parental Tg2576 strain.
What was the basis of lower amyloid in the mice? In brain, staining for the macrophage marker CD45 nearly doubled, and Town observed CD45- and CD11b-positive infiltrating macrophages. The macrophages contained Aβ in vivo, and they showed a higher capacity to phagocytose Aβ in vitro than control cells. From these experiments, Town concluded that getting rid of TGF-βRII signaling removed a negative regulatory influence on the macrophages, allowing them to become activated to clear Aβ. Importantly, the activation was not associated with proinflammatory cytokine production either in vivo or in vitro. The results that shutting down TGF-β signaling in the periphery promotes plaque clearance contrasts with some of Wyss-Coray’s earlier work suggesting that TGF-β production in the brain promotes plaque removal by stimulating microglial uptake (Wyss-Coray et al., 2001). Together, the studies support the idea that macrophage and microglial activation are not just two phenotypes, and show that different approaches to modulating TGF-β action may have very different outcomes. Town concluded by saying that blocking TGF-β immune signaling in the periphery may be a promising therapeutic avenue for AD.—Pat McCaffrey
At this year’s annual meeting of the Society for Neuroscience, a grab bag of studies on the amyloid-β peptide highlighted some outstanding questions about the pesky fragment and its neurotoxic actions. What follows is just a brief flavor of some of the presentations that addressed novel approaches to understanding the ramifications of intracellular Aβ, and how the shapes it assumes, both inside and outside cells, might define its toxicity. One goal in Alzheimer disease (AD) research, of course, is new therapeutic approaches to blocking Aβ toxicity, and some examples of novel vaccination strategies follow here, too.
The Aβ42 peptide comes in a variety of aggregation states, from monomers to small oligomers to fibrils to frank amyloid. In his talk, Koichi Iijima presented data suggesting that changing the intraneuronal aggregation state of Aβ could lead to different patterns of neurotoxicity in his fruit fly model of Aβ accumulation.
When he was with Yi Zhong at Cold Spring Harbor Laboratory in New York, Iijima developed a Drosophila model of AD by overexpressing either Aβ40 or Aβ42 in neurons (see ARF related news story). The flies with Aβ42 had learning deficits, reduced lifespan, amyloid buildup, and neurodegeneration. The flies also showed both plaques and intraneuronal accumulation of Aβ42, mainly in the protein secretory pathway and lysosomes.
Now starting his own lab at Thomas Jefferson University, Philadelphia, Pennsylvania, Iijima is exploring how the aggregation state of Aβ might affect its toxicity. To do this, Iijima and colleagues took the tack of expressing Aβ42 mutants in their Drosophila AD model. They chose the Arctic mutation to increase aggregation, and made a leucine to proline substitution at position 17 to produce a peptide less likely to aggregate.
Their hypothesis was that the different conformations might lead to different phenotypes, and they were right. They found that the Arctic form of Aβ accumulates in neuronal cell bodies and causes cell body degeneration. In contrast, the aggregation-defective mutant appeared mainly in neurites and induced neurite degeneration. Previously, they had shown that wild-type Aβ42 accumulated in both locations.
In addition to neuron loss, the flies developed age-related short-term memory deficits and motor problems, and had a shorter lifespan. All these effects were more pronounced with the Arctic mutation, consistent with its enhanced pathogenicity in people. But the aggregation-deficient Aβ had its own sticking point—it caused greater memory deficits than wild-type Aβ.
Their results show that Aβ42 with different aggregation properties causes distinct behavioral and pathological phenotypes. The coincidence of localization and pathology strengthens the idea that intraneuronal Aβ is the toxic species in this model. Iijima hypothesized that wild-type Aβ may assume different conformations in cells, leading to its own demonstrated multifaceted toxicity.
Generic amyloid as antigen…
Many proteins unrelated to Alzheimer disease show a propensity to aggregate into amyloid structures. Because of this, and from Charlie Glabe’s work with oligomer-reactive antiserum, it has been proposed that peptides of varying primary structure adopt a common toxic oligomeric conformation. To test this idea, Marcelo Vieira, a graduate student working with Sergio Ferreira and Fernanda De Felice at the Federal University of Rio de Janeiro, Brazil, investigated the neurotoxicity of soluble oligomers from one of these unrelated proteins, hen egg white lysozyme (HEWL).
Vieira chose HEWL because the human lysozyme protein is well-known to be amyloidogenic, and variants of it cause hereditary systemic amyloidoses. He showed that under partially denaturing conditions, HEWL formed β-sheet-rich soluble oligomers, which then went on to form fibrils. The oligomers (at 5 uM) were toxic to rat cortical neurons in culture. At higher concentrations (20 uM), the oligomers induced tau phosphorylation at sites associated with AD pathology (Thr212/Ser214 and Ser404). Finally, Vieira showed that injecting the oligomers into the rat cerebral cortex caused neurodegeneration not only in the cortex, but also in the hippocampus, thalamus, and amygdala, as measured by Fluoro-Jade C staining. This effect was not seen with fibrillar preparations of lysozyme or Aβ. An unexpected result was that the HEWL oligomers did not react with a commercially available preparation of the A11 anti-oligomer antiserum, in contrast to Glabe’s original report, which showed that the antiserum reacted with oligomers of human lysozyme (see ARF related news story). Nonetheless, Vieira’s results support the toxic conformation theory.
One corollary of that theory holds that antibodies that can neutralize harmful conformations should be neuroprotective. Using that idea as the basis for a novel vaccine strategy, Becky Stodola, working with Pritam Das and Todd Golde at the Mayo Clinic in Jacksonville, Florida, is testing the use of heterologous amyloids as immunogens to induce an anti-plaque response. The advantage of this approach lies in the use of non-human protein sequences that lower the risk of generating self-reactive antibodies. The structure of amyloid, with its large molecular weight, repetitive structure, and poor clearance and complement activation properties, also means it is more likely to induce a T cell-independent response, which could further reduce unwanted inflammatory reactions. Stodola showed that immunization of mice of various strains with amyloid formed from peptides derived from several adenoviral or bacterial proteins, the yeast prion sup35, or even a butoxycarbonyl dipeptide-induced antiserum that recognized fibrillar Aβ. The antisera have not yet been tested against monomeric or oligomeric Aβ, Stodola said. The group is now working on evaluating the heterologous amyloid vaccines to see if they reduce Aβ deposition in mice.
…Or Oligomer
Taking the passive vaccination approach, Matthew Seager from Merck, West Point, Pennsylvania, presented a poster on Merck’s anti-oligomer antibody development. Working with Grant Krafft at Acumen Pharmaceuticals, South San Francisco, California, they have produced multiple high-affinity, humanized monoclonal antibodies that preferentially recognize soluble Aβ oligomers. The antibodies block oligomer binding to neurons, and their new data showed that weekly administration lowered brain Aβ in mice. Antibodies with therapeutic potential are now in testing for their ability to improve memory and behavior in mice.
Another Merck researcher, Gene Kinney, had a separate presentation on selecting peptides for Aβ immunization. By keeping peptides short (eight or fewer amino acids), Kinney and colleagues hope to avoid triggering T cell responses, which require the presentation of longer peptides. By systematically scanning the entire Aβ sequence with overlapping peptides, they discovered scattered immunogenic sites that were not predicted based on their position in the Aβ sequence. Immunization of Rhesus monkeys with a dual antigen featuring two different peptides conjugated onto one carrier protein produced high levels of amyloid-reactive antibodies in Rhesus monkeys, with no indication of amyloid-specific T cell activation.—Pat McCaffrey.
No Available Comments
No Available Further Reading
A lively platter of slide talks on APP processing and β-secretase (BACE) activities yielded a few interesting tidbits on the localization and regulation of β cleavage at this year’s annual meeting of the Society for Neuroscience in Atlanta, Georgia. The presentations also left the impression that cathepsin B, most recently in the news for digesting fibrillar Aβ (see ARF related news story), may yet have a role to play in the production of Aβ, as a β-secretase candidate protease.
Two talks focused on the localization and fluctuations of the BACE protein in brain. In the first, Matthew Kennedy and colleagues at Schering-Plough Research Institute, Kenilworth, New Jersey, described a radio-labeled small molecule BACE inhibitor that specifically binds BACE in mouse tissues—there was no binding to brains from BACE knockout mice. In brain sections of 6-week-old mice, they detected inhibitor binding throughout the CNS, with higher levels in the CA2/3 regions of the hippocampus and in the olfactory bulb. Using transgenic CRND8-APPswe/ind AD mice that show very early plaque deposition (10-12 weeks of age), they found that BACE levels increase after plaque deposition. In the mice, they saw a 50 percent increase in BACE inhibitor binding only after 24-30 weeks. They also saw a change in localization of the protein to high-staining foci in the cortex, which appear to co-localize with plaques.
The delay in upregulation of BACE is at odds with data presented by Jie Zhao in Robert Vassar’s lab on a new monoclonal antibody they developed to BACE. (See our ARF Madrid story for Vassar’s talk on the antibody, which the lab produced by immunizing BACE knockout mice.) Unlike all commercial antibodies tested, which either recognized multiple proteins on Western blots, or stained the brains of BACE knockout just as well as wild-type mice, the new antibody was monospecific for BACE. Zhao’s immunostaining results revealed increased BACE in the 5XFAD APP/S1 (see ARF related news story) and Tg2576 transgenic mice around amyloid plaques. The BACE elevation occurred in parallel with the rise in amyloid burden in 5XFAD mice. Increases were also seen in brain of human AD patients.
Consistent with the labeled inhibitor experiments of the Schering-Plough group, Zhao showed co-localization of BACE around amyloid plaques. Confocal views revealed BACE in an outer ring of Aβ40 that surrounded the inner, Aβ42-rich plaque. From these and other recent results, Vassar and colleagues hypothesize that energy insufficiency stress, caused, for example, by vascular hypoperfusion, induces an increase in BACE. The subsequent amyloid deposition may itself further activate BACE. Peri-plaque BACE was found in association with neuronal markers.
In a related presentation, Sarah Cole, also at Northwestern, showed some early results from crossing BACE knockouts with the 5XFAD APP/S1 strain. When Cole and colleagues looked at 4-month-old BACE-heterozygous mice, they saw a normalization of early markers of neuronal stress, namely p25 protein and phospho p38 MAP kinase. Until the mice get older, the researchers won’t know if the pathology is actually prevented, or just delayed.
Is BACE the One and Only β-secretase?
The observation that knocking out BACE1 shuts down the constitutive production of Aβ from cultured neurons and the accumulation of Aβ in FAD mouse models has been taken as proof that BACE1 is the predominant enzyme responsible for β cleavage of APP. But is BACE really the only β-secretase? Work presented by Vivian Hook, University of California, San Diego, made a strong case for cathepsin B as an additional β-secretase with a role to play in the activity-regulated secretion of Aβ.
Hook and colleagues have proposed previously that the majority of Aβ is released from cells via regulated secretion, as in the activity-dependent production and release of Aβ at synapses. According to their hypothesis, only a small amount of extracellular Aβ would derive from constitutive secretion, the BACE-dependent pathway through which Aβ makes its way into the conditioned medium of cultured neurons. The researchers, who have long studied the processing and release of neuropeptides, proposed this model based on their studies of adrenal chromaffin cells, which are widely used as a model of regulated secretion of neurotransmitters. In these cells, they have identified cathepsin B as the major β-secretase activity in secretory vesicles. BACE1 is present in the vesicles but accounts for only a small part of the total processing activity during KCl or nicotine-stimulated secretion. From these results, Hook and colleagues have proposed that cathepsin B could be the main β-secretase in neurons (Hook et al., 2002; Hook and Reisine, 2003; Hook et al., 2005).
One reason why cathepsin B has been overshadowed by BACE could be that, as Hook and colleagues demonstrated several years ago, the enzyme prefers to cleave wild-type APP, and displays much lower activity toward the altered site created by the Swedish mutation. The mutant sequence is preferred by BACE, and pops up in many of the FAD animal models which have been used to study the role of BACE in vivo. For studying β-cleavage inhibitors, Hook and coworkers favor the guinea pig model, which has a wild-type APP sequence that matches the β-secretase cleavage site in humans.
Hook used that animal to look at the role of cathepsin B in APP processing in the CNS. In her talk, she showed that infusion of selective cathepsin B inhibitor CA-074Me into the brains of guinea pigs reduced Aβ40 and Aβ42 levels by approximately one-half. In a second talk, Hook showed that another cathepsin B inhibitor, loxistatin, had the same effect after direct intracerebroventricular infusion. She saw decreased production of Aβ and the C-terminal β-secretase fragment of APP in the brain and in isolated synaptosomes. These results suggest that cathepsin B does participate in Aβ production in vivo as a β-secretase, and that inhibitors may have some potential as Aβ-lowering agents. This work is now in press in Biological Chemistry, Hook said.
A listener was quick to ask how Hook could reconcile her results with the recent paper from Li Gan showing that AD mice with the cathepsin B gene knocked out have worse plaque pathology than mice with the enzyme (see ARF related news story). In that study, the researchers found no evidence that cathepsin B acted as a secretase, but in fact found that it was able to degrade Aβ fibrils.
Hook pointed out that the AD mouse model used in that paper (the hAPP J20 line) incorporated the Swedish mutation, which could explain why the researchers saw no evidence for APP processing by cathepsin B. In animals with wild-type human APP, there could be a different outcome. Clearly, there is a lot more work to be done, but the data so far suggest that where Aβ production is concerned, BACE may be just one part of the story.—Pat McCaffrey.
The Alzforum Awards have become an annual ritual to recognize altruism among Alzheimer researchers. Every year, the editors consider the many scientists who have actively contributed to the Alzheimer Research Forum website and select a choice half-dozen who have gone to extra lengths to serve this Web community. We thank each and every one of them for being exemplary members of the Alzforum community. Pat McCaffrey presented the awards at the AD Social at the Society for Neuroscience annual meeting in Atlanta. Awardees received an elegant, engraved Tiffany lead crystal paperweight, suitable for refracting rays of light into the darkest corners of their offices.
The 2006 Alzforum Award recipients are
![]() Sam Gandy, Thomas Jefferson University, Outstanding Contributor, for his leadership in proposing and leading the live discussion Not Dead Yet: Estrogen Deserves Another Chance.
Sam Gandy, Thomas Jefferson University, Outstanding Contributor, for his leadership in proposing and leading the live discussion Not Dead Yet: Estrogen Deserves Another Chance.
![]() Minji Kim, Alice Lu, and Rudy Tanzi of Massachusetts General Hospital, Outstanding Contributors, for composing the detailed eight-part summary of the Keystone Symposia early in 2006:
Minji Kim, Alice Lu, and Rudy Tanzi of Massachusetts General Hospital, Outstanding Contributors, for composing the detailed eight-part summary of the Keystone Symposia early in 2006:
![]() Tobias Hartmann, University of the Saarland, Outstanding Contributor, for his thoughtful commentaries and for generously contributing his time and ideas to guiding Alzforum. See, for example, his comment on the news story AβPP Processing—Limping Along on Lipases.
Tobias Hartmann, University of the Saarland, Outstanding Contributor, for his thoughtful commentaries and for generously contributing his time and ideas to guiding Alzforum. See, for example, his comment on the news story AβPP Processing—Limping Along on Lipases.
![]() Nikolaos Robakis, Mt. Sinai School of Medicine, Outstanding Contributor, for long-time involvement on the Alzforum as an advisor, commentator, and critic who has fearlessly poked holes in the amyloid cascade hypothesis and championed the scientific underdogs. See, for example, Alzheimer Research Forum's 10th Anniversary Symposium: Mapping the Next Decade of Alzheimer Research.
Nikolaos Robakis, Mt. Sinai School of Medicine, Outstanding Contributor, for long-time involvement on the Alzforum as an advisor, commentator, and critic who has fearlessly poked holes in the amyloid cascade hypothesis and championed the scientific underdogs. See, for example, Alzheimer Research Forum's 10th Anniversary Symposium: Mapping the Next Decade of Alzheimer Research.
![]() John Morris, Washington University St. Louis, merited the Mensch Award for selflessly providing much valuable advice and participation in live discussions and interviews, and for posting the Antecedent Biomarkers for AD workshop proceedings. See interview.
John Morris, Washington University St. Louis, merited the Mensch Award for selflessly providing much valuable advice and participation in live discussions and interviews, and for posting the Antecedent Biomarkers for AD workshop proceedings. See interview.
![]() Dean Hartley, Rush University Medical Center, received the Vision Award 2006 for being one of our earliest and most creative alpha testers, whose suggestions over the years have led to countless improvements of the Alzforum, including the Antibody Directory. He has also been deeply involved in the creation of SWAN (Semantic Web Applications in Neuromedicine), an innovative knowledge management technology that ARF members will be hearing more about next year....
Dean Hartley, Rush University Medical Center, received the Vision Award 2006 for being one of our earliest and most creative alpha testers, whose suggestions over the years have led to countless improvements of the Alzforum, including the Antibody Directory. He has also been deeply involved in the creation of SWAN (Semantic Web Applications in Neuromedicine), an innovative knowledge management technology that ARF members will be hearing more about next year....
No Available Comments
No Available Further Reading
In neurons, APP-laden vesicles powered by kinesin motors ride from the cell body out to synapses. But is APP just a passenger, or does the protein sit in the driver’s seat? New work from Elaine Bearer of Brown University in Providence, Rhode Island, and the Marine Biological Laboratory at Woods Hole, Massachusetts, suggests the latter. In a study presented this month at the 36th annual meeting of the Society for Neuroscience (SfN) in Atlanta, Georgia, and published shortly thereafter in the October 24 PNAS online, Bearer and lead authors Prasanna Satpute-Krishnan, Joseph DeGiorgis and Michel Conley show that a 15 amino acid C-terminal peptide from human APP can recruit cargoes of synthetic beads to the fast axonal transport (FAT) machinery in squid giant axons. The results suggest that one physiological function of APP could be to direct axonal transport of vesicles or other cargoes, a process known to be compromised in Alzheimer disease (for a recent review see Stokin and Goldstein, 2006).
The squid giant axon was also on display at another presentation at the SfN meeting, this one by Gustavo Pigino from Scott Brady’s lab at the University of Illinois in Chicago. Following up on recent work showing that polyglutamate-expanded proteins inhibit FAT in extruded squid axoplasm (see ARF related news story), Pigino showed that Aβ peptide oligomers inhibit both anterograde and retrograde transport in the same system, an effect they attributed to Aβ’s activation of casein kinase II.
APP first came to the notice of Bearer and colleagues in their studies on the transport of herpes simplex virus (HSV) in neurons. The virus moves from cell body to synapse via kinesin-powered FAT. When the Brown researchers injected purified human HSV particles into isolated squid giant axons, they could reconstitute this transport, and found that the transported virus contained high amounts of human APP (see ARF related news story). APP has been implicated as a motor receptor in vesicle movement by the work of Lawrence Goldstein and others (see Kamal et al., 2000 and ARF related news story), leading Bearer to hypothesize a similar role for APP in virus transport.
This is where the study gets colorful. Rather than follow the movement of virus particles, which contain other proteins and lipids in addition to APP, the researchers decided to simplify the system. They replaced the virus with similarly sized fluorescent polystyrene beads to which they coupled defined peptides. This allowed them to test sequence requirements for transport. In this system, video microscopy of injected beads derivatized with a peptide corresponding to the last 15 amino acids of the C-terminal cytoplasmic tail of APP revealed a rapid, unidirectional anterograde transport. The speed of movement was consistent with FAT, and comparable to that seen for endogenous organelles or intact virus in the same system. The transport function was specific to the C-terminal peptide, because in the same axons, different color beads coupled to a peptide derived from the extracellular domain of APP, or a scrambled C-terminal sequence, displayed no motility at all (see movie below).
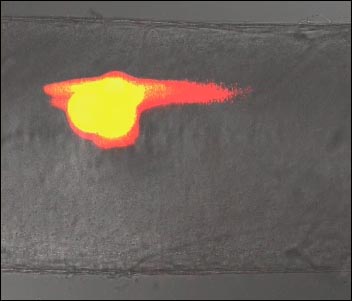
APP C-terminal Drives Fast Axonal Transport
Fluorescent virus-sized particles coupled to the C-terminal (red) of APP drive fast anterograde transport when injected into the squid giant axon, while particles coupled to the N-terminal of APP (green) remain stationary. The movie and the paper are available as open access on the PNAS website. [Image courtesy PNAS]
The function of APP in transport appears to be highly conserved. Cloning of squid APP revealed a nearly identical C-terminal sequence (13 out of 15 amino acid match to the human), and transport studies showed that the squid cytoplasmic domain also supported bead transport. In further support for a physiological role of APP in transport, the researchers demonstrated that the intact C99 fragment of human APP, consisting of a small luminal/extracellular stretch, plus the transmembrane and cytoplasmic domain, could mediate transport when conjugated to beads at a similar density as found on HSV. Transport of beads coupled to either C99 or the C-terminal peptide was blocked by addition of excess free peptide, suggesting that the protein was binding specifically to some part of the motor assembly.
The results support the idea that APP is involved in HSV transport in neurons, and raises the possibility that it could play a wider role in recruitment of the transport machinery for anterograde shipments in general. The domain contains an NPXY motif which participates in many protein-protein interactions, and could contact kinesin directly, as Goldstein has proposed, or via a scaffolding protein (Taru et al., 2002). Bearer and colleagues call the short peptide a “zipcode” for anterograde transport, but while the sequence is sufficient for transport, further work will be required to show if it is necessary.
Gustavo Pigino also showed data on FAT in the squid axon, where he and his colleagues are studying the effects of Aβ oligomers. Like Bearer, Brady and colleagues summer in Woods Hole, where they study axonal transport not in intact axons, but in extruded axoplasm preparations. Because they have removed the plasma membrane barrier, their system allows them to add proteins or inhibitors directly to cytosolic transport machinery, and look for effects on anterograde or retrograde transport and the motor proteins involved. Earlier this year, they showed that polyglutamine-expanded androgen receptor inhibits FAT by turning on jun N-terminal kinase, a regulator of kinesin activity (see ARF related news story).
In his talk, Pigino described similar experiments testing the effects of Aβ—soluble, oligomeric, or fibrillar. Only oligomeric Aβ inhibited transport at very low concentrations (100 nM), and it slowed movement in both anterograde and retrograde directions. Addition of active casein kinase II (CKII) mimicked the effect of Aβ, suggesting that the oligomers were causing activation of this enzyme. Consistent with these results, Aβ oligomers increased phosphorylation of the CKII substrate kinesin light chain, while addition of a CKII inhibitor along with Aβ restored transport. One attendee raised the issue of whether Aβ oligomers are present in the cytoplasm of neurons in sufficient amounts to elicit these effects in intact cells, a question which remains to be answered for both normal and AD brain.—Pat McCaffrey
Comments
No Available Comments
Make a Comment
To make a comment you must login or register.