Genetic Findings Link Parkinson’s to Crohn’s Disease, Inflammation
Quick Links
Researchers are finding links between Parkinson’s disease and the gut, and a new genetic study ties the two even closer together. In the January 10 Science Translational Medicine, researchers led by Inga Peter and Judy Cho at Icahn School of Medicine at Mount Sinai, New York, report that several variants in the LRRK2 gene raise or lower risk not only for PD but also for Crohn’s disease, an inflammatory bowel disorder. In particular, the researchers identified a new functional risk variant, N2081D, which boosts LRRK2’s kinase activity, as well as a protective variant that inactivates LRRK2. The findings may provide insight into underlying disease mechanisms and point toward therapeutic approaches, Peter said. For example, LRRK2 inhibitors being developed for PD might help people with Crohn’s disease, while anti-inflammatory approaches could benefit Parkinson’s patients, she suggested.
- A genetic study identified N2081D and R1398H in the LRRK2 gene as risk and protective factors, respectively, for Crohn’s disease.
- Both variants also affect Parkinson’s risk in the same way.
- The findings hint that common disease mechanisms may underlie both disorders.
Other researchers agreed the paper may open up new research avenues. “These data tell us that Parkinson’s is, at least in part, an inflammatory disease,” said Mark Cookson at the National Institutes of Health in Bethesda, Maryland. He added that the findings need to be replicated in large Parkinson’s cohorts.
In 2003, neuroanatomists Heiko Braak and Kelly Del Tredici proposed the controversial idea that an infection in the gut or nose could kick off inflammation and α-synuclein pathology that spreads to the brain (Jul 2011 news series). The idea of a gut-PD link has gained ground, and recently researchers reported changes in intestinal microbiota in early PD, which may accelerate α-synuclein pathology (Dec 2016 news; Apr 2017 news). Crohn’s disease had not been directly linked to PD, although it does associate with variants in the LRRK2 locus (Barrett et al., 2008; Franke et al., 2010; Jostins et al., 2012). These are distinct from the LRRK2 variants, such as G2019S, that predispose people to familial or sporadic PD.

LRRK2 Pleiotropy.
Some variants of this large multifunctional protein elevate or dampen risk for both Parkinson’s and Crohn’s disease. [Courtesy of Science Translational Medicine/AAAS.]
Peter and Cho study Crohn’s disease, and they wanted to find new genetic risk factors that might guide the development of treatments. First author Ken Hui at Yale University School of Medicine, New Haven, Connecticut, combed through exome-sequencing data from 50 people who had Crohn’s disease and were of Ashkenazi Jewish heritage. This population is particularly susceptible to Crohn’s. Hui identified 4,277 new coding variants, which he added to an existing exome chip that queries 230,296 variants in more than 20,000 genes. The authors then used the chip to identify disease associations in 1,477 people with Crohn’s and 2,614 healthy controls, finding three loci with chip-wide significance. Two were known risk factors for Crohn’s, but the third, LRRK2, surprised them. It contained two strong signals: the new variant N2081D, which associated with a nearly twofold higher risk of Crohn’s, and N551K, which correlated with lower risk. N551K and the nearby variants K1423K and R1398H had been reported previously to be inherited together as a protective haplotype for PD (Ross et al., 2011).
The findings suggested to the authors that Crohn’s disease and PD might share some risk factors. To test this idea, they expanded the association study to a total of 6,538 Crohn’s cases and 12,607 healthy controls, and added 5,570 PD cases for comparison. About one-third of this cohort was of Ashkenazi Jewish heritage. As before, N2081D emerged as a strong risk factor for Crohn’s, with an odds ratio of about 1.6. N2081D bumped up PD risk as well, with an odds ratio of 1.3. The protective N551K/R1398H haplotype lowered risk for both diseases, with odds ratios ranging from 0.67 to 0.89. These represent the first coding variants to be linked to both PD and Crohn’s, Cookson noted. The effect of the variants was similar among Jewish and non-Jewish participants, but N2081D was more common in the Ashkenazi Jewish than the general population, with an allele frequency of 8 versus 3 percent.
What does N2081D do? The authors first turned up evidence that this polymorphism accounts for most of the previously reported Crohn’s risk in the LRRK2 locus. When they removed people with N2081D from the genetic analysis, the risk associated with other variants disappeared, suggesting it represented the functional variant. Intriguingly, N2081D resides in the same kinase domain as the major PD risk factor, G2019S. Despite their close spatial occurrence, the two variants exerted independent genetic effects and were not inherited together.
Because G2019S is known to ramp up kinase activity, the authors compared the ability of the two variants to phosphorylate a substrate in cell-free experiments (Nov 2005 news). Both N2081D and G2019S bumped up phosphorylation by about 30 percent, indicating similar mechanisms of action. “N2081D is the first functional LRRK2 variant for Crohn’s risk to be identified,” Peter said.
However, the biological effects of N2081D and G2019S are not identical. The former heightens risk for Crohn’s more than PD, while the latter is primarily a PD risk factor with a weak association with Crohn’s as well. Why this difference? Peter believes it may have to do with the substrates LRRK2 interacts with in the cell types most affected in each disease. In the gut, LRRK2 is expressed primarily by macrophages and Paneth cells, specialized epithelial cells of the small intestine that secrete antimicrobial peptides. In this environment, LRRK2 may interact primarily with bacterial peptidoglycans, Peter speculated. In the brain, LRRK2 expression is highest in microglia, and the protein is more likely to phosphorylate brain glycolipids, she added. Thus, the variants may have distinct effects on each substrate.
What about the protective haplotype? Neither the N551K nor R1398H variants affected LRRK2 substrate phosphorylation. However, R1398H occurs in the ROC domain of LRRK2, which helps hydrolyze bound GTP, thereby inactivating the protein. Transfected cells expressing R1398H LRRK2 had more inactive LRRK2 than did those with N551K, N2081D, or G2019S variants. In other words, R1398H switched LRRK2 off. This agrees with a previous report on the variant’s mechanism of action and suggests R1398H represents the functional protective polymorphism (Nixon-Abell et al., 2016). Notably, less-efficient GTP hydrolysis, which keeps LRRK2 on, has been linked to a higher risk of PD (Liao et al., 2014).
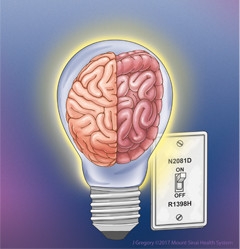
LRRK2 Switch.
The variants N2081D and R1398H exert opposing effects on LRRK2, in effect turning the protein on or off, respectively, in both the brain and gut. [Courtesy of Inga Peter and J. Gregory.]
The linkage between Parkinson’s and Crohn’s was not limited to N2081D and R1398H. The authors analyzed additional independent variants in the LRRK2 gene that showed up in their large association study. These were weaker signals that did not meet exome chip-wide significance, but associated with both Crohn’s and PD. For 25 out of 29 variants, the risk of Crohn’s and PD moved in the same direction, strengthening the idea that LRRK2 acts similarly in the two disorders.
If Crohn’s and PD share risk factors, the diseases should be more likely to occur together. This is supported by a recent Taiwanese population study of 23 million people that found an increased risk of Parkinson’s in people with Crohn’s disease (Lin et al., 2016). Dana Philpott at the University of Toronto, who studies Crohn’s, told Alzforum that researchers had not previously noticed any increase in Parkinson’s in people with the intestinal disorder. Perhaps because the risk variant is rare, the effect is only visible at the population level, she noted. Peter suggested N2081D could be used to screen people with Crohn’s to find those most at risk of PD.
The finding of shared genetic risk intrigued Michael Schlossmacher at Ottawa Hospital Research Institute, Canada. He noted that LRRK2 variants have been linked not only to PD and Crohn’s, but also to leprosy (Mar 2013 conference news). The latter two diseases are both marked by excessive inflammation. In addition, LRRK2 expression in innate immune cells dwarfs that in neurons (Hakimi et al., 2011).
“Maybe LRRK2’s primary role in Parkinson’s is also to regulate inflammation,” Schlossmacher suggested. He recently reported that α-synuclein has antimicrobial effects, while others have found that gut infections stimulate release of α-synuclein (May 2017 news; Jul 2017 news). The data support the idea that PD might result from the long-term consequences of a transient infection that touches off chronic inflammation and α-synuclein accumulation in people with certain genetic susceptibilities, Schlossmacher said. He is currently testing the idea in mouse models.
Previous studies have turned up evidence along these lines (Oct 2008 news; Aug 2009 news; Oct 2016 news). Rudolph Tanzi and Robert Moir at Massachusetts General Hospital, Charlestown, have advanced a similar hypothesis for Alzheimer’s disease (Apr 2009 conference news; Feb 2011 webinar; May 2016 conference news).—Madolyn Bowman Rogers
References
Alzpedia Citations
Series Citations
News Citations
- Do Microbes in the Gut Trigger Parkinson’s Disease?
- Rumblings of Parkinson’s: Gut Microbiome Shifts in Early Stage of Disease
- More Than a Lark? PD Mutations Increase Kinase Activity
- LRRK Watchers’ Eyes Turn to Inflammation, Autophagy, Kinase
- Olfactory System Model Explores Antimicrobial Role for α-Synuclein
- Put ’Em Up: Does α-Synuclein Help Fight Microbes in the Gut?
- Peripheral Inflammation Exacerbates CNS Dysfunction
- Bugs on the Brain—Can Flu Cause Parkinsonism, Neurodegeneration?
- Could Bacterial Amyloid Trigger Parkinson’s Pathology?
- Prague: Aβ Rehabilitated as an Antimicrobial Protein?
- Microbial Hypotheses Intrigue at Zilkha Alzheimer’s Meeting
Webinar Citations
Paper Citations
- Barrett JC, Hansoul S, Nicolae DL, Cho JH, Duerr RH, Rioux JD, Brant SR, Silverberg MS, Taylor KD, Barmada MM, Bitton A, Dassopoulos T, Datta LW, Green T, Griffiths AM, Kistner EO, Murtha MT, Regueiro MD, Rotter JI, Schumm LP, Steinhart AH, Targan SR, Xavier RJ, NIDDK IBD Genetics Consortium, Libioulle C, Sandor C, Lathrop M, Belaiche J, Dewit O, Gut I, Heath S, Laukens D, Mni M, Rutgeerts P, Van Gossum A, Zelenika D, Franchimont D, Hugot JP, de Vos M, Vermeire S, Louis E, Belgian-French IBD Consortium, Wellcome Trust Case Control Consortium, Cardon LR, Anderson CA, Drummond H, Nimmo E, Ahmad T, Prescott NJ, Onnie CM, Fisher SA, Marchini J, Ghori J, Bumpstead S, Gwilliam R, Tremelling M, Deloukas P, Mansfield J, Jewell D, Satsangi J, Mathew CG, Parkes M, Georges M, Daly MJ. Genome-wide association defines more than 30 distinct susceptibility loci for Crohn's disease. Nat Genet. 2008 Aug;40(8):955-62. Epub 2008 Jun 29 PubMed.
- Franke A, McGovern DP, Barrett JC, Wang K, Radford-Smith GL, Ahmad T, Lees CW, Balschun T, Lee J, Roberts R, Anderson CA, Bis JC, Bumpstead S, Ellinghaus D, Festen EM, Georges M, Green T, Haritunians T, Jostins L, Latiano A, Mathew CG, Montgomery GW, Prescott NJ, Raychaudhuri S, Rotter JI, Schumm P, Sharma Y, Simms LA, Taylor KD, Whiteman D, Wijmenga C, Baldassano RN, Barclay M, Bayless TM, Brand S, Büning C, Cohen A, Colombel JF, Cottone M, Stronati L, Denson T, De Vos M, D'Inca R, Dubinsky M, Edwards C, Florin T, Franchimont D, Gearry R, Glas J, Van Gossum A, Guthery SL, Halfvarson J, Verspaget HW, Hugot JP, Karban A, Laukens D, Lawrance I, Lemann M, Levine A, Libioulle C, Louis E, Mowat C, Newman W, Panés J, Phillips A, Proctor DD, Regueiro M, Russell R, Rutgeerts P, Sanderson J, Sans M, Seibold F, Steinhart AH, Stokkers PC, Torkvist L, Kullak-Ublick G, Wilson D, Walters T, Targan SR, Brant SR, Rioux JD, D'Amato M, Weersma RK, Kugathasan S, Griffiths AM, Mansfield JC, Vermeire S, Duerr RH, Silverberg MS, Satsangi J, Schreiber S, Cho JH, Annese V, Hakonarson H, Daly MJ, Parkes M. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn's disease susceptibility loci. Nat Genet. 2010 Dec;42(12):1118-25. PubMed.
- Jostins L, Ripke S, Weersma RK, Duerr RH, McGovern DP, Hui KY, Lee JC, Schumm LP, Sharma Y, Anderson CA, Essers J, Mitrovic M, Ning K, Cleynen I, Theatre E, Spain SL, Raychaudhuri S, Goyette P, Wei Z, Abraham C, Achkar JP, Ahmad T, Amininejad L, Ananthakrishnan AN, Andersen V, Andrews JM, Baidoo L, Balschun T, Bampton PA, Bitton A, Boucher G, Brand S, Büning C, Cohain A, Cichon S, D'Amato M, De Jong D, Devaney KL, Dubinsky M, Edwards C, Ellinghaus D, Ferguson LR, Franchimont D, Fransen K, Gearry R, Georges M, Gieger C, Glas J, Haritunians T, Hart A, Hawkey C, Hedl M, Hu X, Karlsen TH, Kupcinskas L, Kugathasan S, Latiano A, Laukens D, Lawrance IC, Lees CW, Louis E, Mahy G, Mansfield J, Morgan AR, Mowat C, Newman W, Palmieri O, Ponsioen CY, Potocnik U, Prescott NJ, Regueiro M, Rotter JI, Russell RK, Sanderson JD, Sans M, Satsangi J, Schreiber S, Simms LA, Sventoraityte J, Targan SR, Taylor KD, Tremelling M, Verspaget HW, De Vos M, Wijmenga C, Wilson DC, Winkelmann J, Xavier RJ, Zeissig S, Zhang B, Zhang CK, Zhao H, International IBD Genetics Consortium (IIBDGC), Silverberg MS, Annese V, Hakonarson H, Brant SR, Radford-Smith G, Mathew CG, Rioux JD, Schadt EE, Daly MJ, Franke A, Parkes M, Vermeire S, Barrett JC, Cho JH. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012 Nov 1;491(7422):119-24. PubMed.
- Ross OA, Soto-Ortolaza AI, Heckman MG, Aasly JO, Abahuni N, Annesi G, Bacon JA, Bardien S, Bozi M, Brice A, Brighina L, Van Broeckhoven C, Carr J, Chartier-Harlin MC, Dardiotis E, Dickson DW, Diehl NN, Elbaz A, Ferrarese C, Ferraris A, Fiske B, Gibson JM, Gibson R, Hadjigeorgiou GM, Hattori N, Ioannidis JP, Jasinska-Myga B, Jeon BS, Kim YJ, Klein C, Kruger R, Kyratzi E, Lesage S, Lin CH, Lynch T, Maraganore DM, Mellick GD, Mutez E, Nilsson C, Opala G, Park SS, Puschmann A, Quattrone A, Sharma M, Silburn PA, Sohn YH, Stefanis L, Tadic V, Theuns J, Tomiyama H, Uitti RJ, Valente EM, van de Loo S, Vassilatis DK, Vilariño-Güell C, White LR, Wirdefeldt K, Wszolek ZK, Wu RM, Farrer MJ, Genetic Epidemiology Of Parkinson's Disease (GEO-PD) Consortium. Association of LRRK2 exonic variants with susceptibility to Parkinson's disease: a case-control study. Lancet Neurol. 2011 Oct;10(10):898-908. Epub 2011 Aug 30 PubMed.
- Nixon-Abell J, Berwick DC, Grannó S, Spain VA, Blackstone C, Harvey K. Protective LRRK2 R1398H Variant Enhances GTPase and Wnt Signaling Activity. Front Mol Neurosci. 2016;9:18. Epub 2016 Mar 8 PubMed.
- Liao J, Wu CX, Burlak C, Zhang S, Sahm H, Wang M, Zhang ZY, Vogel KW, Federici M, Riddle SM, Nichols RJ, Liu D, Cookson MR, Stone TA, Hoang QQ. Parkinson disease-associated mutation R1441H in LRRK2 prolongs the "active state" of its GTPase domain. Proc Natl Acad Sci U S A. 2014 Mar 18;111(11):4055-60. Epub 2014 Mar 3 PubMed.
- Lin JC, Lin CS, Hsu CW, Lin CL, Kao CH. Association Between Parkinson's Disease and Inflammatory Bowel Disease: a Nationwide Taiwanese Retrospective Cohort Study. Inflamm Bowel Dis. 2016 May;22(5):1049-55. PubMed.
- Hakimi M, Selvanantham T, Swinton E, Padmore RF, Tong Y, Kabbach G, Venderova K, Girardin SE, Bulman DE, Scherzer CR, LaVoie MJ, Gris D, Park DS, Angel JB, Shen J, Philpott DJ, Schlossmacher MG. Parkinson's disease-linked LRRK2 is expressed in circulating and tissue immune cells and upregulated following recognition of microbial structures. J Neural Transm (Vienna). 2011 May;118(5):795-808. Epub 2011 May 7 PubMed.
Further Reading
Primary Papers
- Hui KY, Fernandez-Hernandez H, Hu J, Schaffner A, Pankratz N, Hsu NY, Chuang LS, Carmi S, Villaverde N, Li X, Rivas M, Levine AP, Bao X, Labrias PR, Haritunians T, Ruane D, Gettler K, Chen E, Li D, Schiff ER, Pontikos N, Barzilai N, Brant SR, Bressman S, Cheifetz AS, Clark LN, Daly MJ, Desnick RJ, Duerr RH, Katz S, Lencz T, Myers RH, Ostrer H, Ozelius L, Payami H, Peter Y, Rioux JD, Segal AW, Scott WK, Silverberg MS, Vance JM, Ubarretxena-Belandia I, Foroud T, Atzmon G, Pe'er I, Ioannou Y, McGovern DP, Yue Z, Schadt EE, Cho JH, Peter I. Functional variants in the LRRK2 gene confer shared effects on risk for Crohn's disease and Parkinson's disease. Sci Transl Med. 2018 Jan 10;10(423) PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Indiana University School of Medicine
Regarding the paper by Hui et al., LRRK2 was implicated in inflammation and specifically Crohn's disease about half a decade ago. It is interesting and novel that they have identified N2081D as a risk factor for Crohn's disease and R1398H as a protective mutant.
On the potential connection between Parkinson’s disease etiology and that of the gut, the authors reasoned that since N2081 resides within the kinase domain of LRRK2, as does the Parkinson's disease-associated mutation G2019S, it might also affect the kinase activity of LRRK2 in similar ways. This is a reasonable initial hypothesis, however, residue G2019 resides precisely in the active site of LRRK2 (based on a homology model) and residue N2081 resides in the distal side of the C-lobe, which is far away from the active site and pointing into the solvent, rendering it unlikely to have any direct effects on the active site or substrate-binding site of LRRK2. However, in the western blot assay showing that N2018D increased phosphorylation of Rab10 (figure 4B), the difference in activity between N2018D LRRK2 and that of WT is small (less than 0.5), and western blots are prone to sample-to-sample variability in that range.
Likewise, in the GTPase activity assay (figure 4C) R1398H LRRK2 activity is only slightly higher than that of WT (less than 0.5) and the TLC assay, due to smearing effects and high background, is prone to high background errors.
Overall, the paper raises an interesting possibility that Crohn's disease and Parkinson's disease might potentially share the same pathogenic mechanism; however, this would need to be confirmed with additional evidence.
Make a Comment
To make a comment you must login or register.