Single Synapse Mass Spec Snags CD47 as Alzheimer’s Resilience Factor
Quick Links
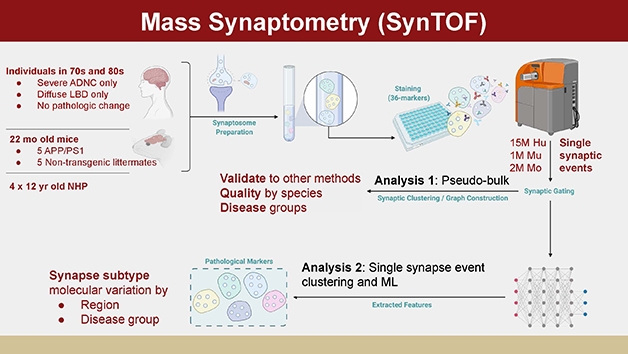
The study of synapses presents a problem: Researchers can either peer up-close at single synapses, missing the big picture, or capture a bird’s-eye view of thousands of these tiny structures, missing detail. A new technique, flow cytometry with time-of-flight mass spectrometry, aka SynTOF, offers a solution that marries detail with quantity. Developed by Thomas Montine at Stanford University in Palo Alto, California, SynTOF enables scientists to examine millions of synapses one at a time, surveying dozens of proteins in each.
- Combining flow cytometry and time-of-flight mass spec, scientists surveyed millions of single synapses.
- In AD brain, high CD47 and low ApoE emerged as protective.
- AD synapses contained little Aβ, belying findings from mouse models of amyloidosis.
In the December 17 Science Advances, Montine and colleagues describe how they applied SynTOF to postmortem human brain, finding differences between synapses in pure Alzheimer’s or Lewy body disease, and those in age-matched healthy tissue. As expected, AD synapses contained a high amount of pathological tau but, to the authors’ surprise, almost no Aβ. This contrasts with findings from mouse models of amyloidosis, which show synapses awash with the peptide.
In addition, the data highlighted high CD47 and low ApoE as being linked to synaptic survival and cognitive resilience in AD. Intriguingly, CD47 functions as a “don’t eat me” signal for microglia, and ApoE as the opposite. “This signaling may be important for the survival of synapses in the presence of AD pathology,” Montine told Alzforum. Some of these data were previously presented at AAIC 2020 (Aug 2020 conference news).
(Courtesy of Montine lab, Stanford University.)
Other researchers were enthusiastic. Randall Bateman at Washington University in St. Louis called the methodology cutting-edge, and noted, “It offers a new orthogonal window to peer into the molecular machinery of AD, and has interesting findings of candidate proteins that may have mechanistic importance at the synapse.” Nicholas Seyfried at Emory University, Atlanta, compared the technique to single-nuclei RNA-Seq, suggesting that SynTOF would be similarly useful for molecular characterization and subtyping. Jürgen Götz at the University of Queensland in Brisbane, Australia, called the approach elegant. “I am convinced this methodology will be widely adopted,” Götz wrote to Alzforum (comments below).
Mass Spec for Synapses
Previous methods of studying synapses analyzed bulk data from homogenized brain, homed in on a few synapses with high-resolution microscopy, or employed two to three antibody probes to detect key proteins in large numbers of synapses via flow cytometry or array tomography. No existing technique allows for a broad protein survey of single synapses at large scale.
To achieve this, Montine turned to cytometry by time-of-flight mass spectrometry (CyTOF), a technique used on cells (Cheung and Utz, 2011; Bendall et al., 2012). In CyTOF, cells are labeled with antibody probes conjugated to different heavy metals and then passed through a nebulizer one at a time into the mass spectrometer, where they are vaporized into atoms. The machine reads the unique mass-to-charge signature of the heavy metal ions to profile the target proteins that were present in each cell. The authors previously adapted this technique to measure synaptosomes, membrane-bound bubbles of mostly presynaptic material isolated from homogenized brain (Gajera et al., 2019; Gajera et al., 2021).
In the new study, joint first authors Thanaphong Phongpreecha and Chandresh Gajera isolated synaptosomes from human brains that met strict criteria for either pure AD pathology, pure Lewy bodies, or no pathology, and had a postmortem interval of less than eight hours. Out of an original cohort of 113 brains, they ended up with nine AD, six Lewy body, and six controls that met these criteria. The researchers took samples from three brain regions—Brodmann’s area 9 in the dorsolateral prefrontal cortex, the hippocampus, and the caudate—isolating a total of 15 million synaptosomes containing presynaptic material, and 820,000 containing postsynaptic.
The authors probed these synaptosomes with a suite of 38 antibodies. Four were used to weed out contaminating nonsynaptic material, 14 to determine neuronal subtype, six to flag cellular injury markers, and three to highlight metabolic markers. Of the remaining 11, five antibodies recognized AD risk factors—Aβ40, Aβ42, paired helical filaments of tau, ApoE, and BIN1—while six detected risk factors for Parkinson’s disease, a Lewy body disorder. These were parkin, GBA1, LRRK2, DJ1, TMEM230, and α-synuclein phosphorylated at residue 129. Heavy metal-labelled antibodies were used for detection because mass spec is limited in the number of different proteins it can distinguish at one time, particularly if they are not abundant.
The Synaptic Signature of AD
Only a few antibodies found differences between AD and control brain. As expected from previous array tomography studies, 18 percent of AD hippocampal presynapses contained PHF-tau, about six times the number in control brain. Less expected was the dearth of DJ1 in AD cortical presynapses, with about half as many containing the protein as in control brain. However, previous studies have found that this stress response protein becomes oxidized during neurodegeneration, leading it to aggregate and form deposits in the frontal cortices of AD and PD patients (Choi et al., 2006; Baulac et al., 2009). Possibly, this aggregation depletes synaptic DJ1, Montine suggested. Notably, the combination of high hippocampal PHF-tau and low cortical DJ1 cleanly separated AD from control brain.
What about Aβ? Surprisingly, only about 2 percent of AD synapses contained Aβ42, the same percentage as in control brain. To make sure the SynTOF technique was able to detect the peptide, the authors analyzed synapses from 22-month-old PS/APP mice and confirmed they were loaded with Aβ. “That says synapses in these mice are quite different from the human condition,” Montine said.
Others disputed this. “It is surprising they do not observe Aβ in human synapses from AD patient brain, as we and others have observed this using multiple methods, including high-resolution imaging and biochemical enrichment of synaptic fractions,” Tara Spires-Jones at the University of Edinburgh wrote to Alzforum (full comment below). She wondered if the Aβ antibodies used for SynTOF might have missed oligomeric Aβ.
Robert Vassar at Northwestern University, Chicago, had a different explanation, noting that postmortem AD brains represent end-stage disease, whereas amyloidosis mice are believed to model an earlier timepoint. “Hence, the PS/APP mouse synapses were actively producing Aβ because the disease process was active and had not yet become end-stage and burned out,” he suggested (full comment below). Montine said the nine AD brains in his study encompassed a range of pathologies, and the cohort included people whose cognition had been relatively preserved at death. “It’s theoretically possible the mice were at a different stage than humans, but I doubt it,” Montine told Alzforum.
The SynTOF findings made sense to Jochen Herms at Ludwig-Maximilians University in Munich. He noted that synaptic pathology in mice occurs close to amyloid plaques, whereas in people synaptic dysfunction associates with tau pathology and often happens far away from plaques. “So I would not expect similar results when comparing synaptosomes from mouse amyloid models and humans with AD-related pathology,” he wrote (comment below).
What Bolsters Resilience?
For Montine, the most interesting finding from AD samples was CD47, an immune receptor. Often associated with cancer, CD47 has been little studied in the brain. Surprisingly, it popped up in all human presynapses analyzed by SynTOF, but was particularly prominent in those with elevated PHF-tau. Why is this important? Previous work had identified CD47, and its receptor SIRPa, as a deterrent to microglial phagocytosis, helping preserve synapses during developmental pruning and possibly neurodegeneration (Lehrman et al., 2018; Ding et al., 2021). Montine believes the high amount of CD47 may have helped the tau-filled synapses persist. “Degeneration has occurred in these brains, and these are the surviving synapses,” he said.
The study gleaned more clues to what protects synapses. Two of the nine people with AD pathology did not have dementia, indicating some resilience against the disease. Although the authors did not see a strong difference in their synapses compared to the other seven AD brains, analyzing those seven alone revealed that ApoE was elevated in their hippocampal synapses compared to control synapses. Taken together, the findings suggest a relative dearth of ApoE hippocampal synapses in the resilient brains. ApoE depletion has been shown previously to keep microglia from gobbling up synapses in tauopathy mice (Wang et al., 2021). “One way to put these different pieces of data together is that surviving synapses have a higher ‘don’t eat me’ and a lower ‘eat me’ signal,” Montine said.
Few previous studies have searched for proteins associated with synaptic resilience. One that did turned up the synaptic proteins VEGF, SMOC1, and NPTX2 as protective, but not CD47 or ApoE (Aug 2019 conference news). On the other hand, Spires-Jones noted that the CD47 data matched her findings from bulk proteome analysis of human synapses (Hesse et al., 2019).
Knowledge Gaps and Frontiers
Like the AD brains, the Lewy body cohort produced both expected and unexpected results. In the former category, about half as many synapses from Lewy body brains as controls contained dopamine transporter, indicating a loss of dopaminergic neurons. In the latter, SynTOF detected no increase in synaptic p129-α-synuclein in Lewy body brains, in conflict with a previous study (Colom-Cadena et al., 2017). This form of α-synuclein misfolds more readily and is associated with PD.
In future work, Montine plans to study brains with mixed pathology, including vascular pathology. He wants to compare those findings to the data from samples with AD and Lewy body pathology to learn how different types of disease burden affect synapses. Mark Cookson at the National Institute on Aging in Bethesda, Maryland, thinks SynTOF should be applied to a range of neurodegenerative diseases. “It would be really interesting to see which changes in disease are specific to AD, and which are general to damaged synapses,” he wrote (comment below).
Commenters noted some limitations of SynTOF. Roberto Malinow at the University of California, San Diego, pointed out that many synaptic changes in AD, such as a loss of PSD-95, occur at the postsynapse and would be missed by this analysis. “I don’t know of a biochemical preparation that contains primarily postsynaptic proteins,” he wrote (comment below). For his part, Vassar wondered if SynTOF could be adapted to study other parts of the neuron, for example axons or dendrites, or organelles like lysosomes.
Götz noted that the results from SynTOF depend on the quality of the antibodies used, and suggested combining multiple antibodies against the same target to get more rigorous data. Seyfried agreed antibody quality is crucial, and also highlighted tissue preparation as a critical factor, noting how few brains met the standard for analysis in this study. “Better cryopreservation techniques could potentially be key to advancing this exciting approach,” Seyfried wrote.—Madolyn Bowman Rogers
References
News Citations
- Seeing into the Human Synapse: New Tools Illuminate Alzheimer’s Hot Spot
- Proteomics Uncovers Potential Markers, Subtypes of Alzheimer’s
Research Models Citations
Paper Citations
- Cheung RK, Utz PJ. Screening: CyTOF-the next generation of cell detection. Nat Rev Rheumatol. 2011 Jul 26;7(9):502-3. PubMed.
- Bendall SC, Nolan GP, Roederer M, Chattopadhyay PK. A deep profiler's guide to cytometry. Trends Immunol. 2012 Jul;33(7):323-32. Epub 2012 Apr 2 PubMed.
- Gajera CR, Fernandez R, Postupna N, Montine KS, Fox EJ, Tebaykin D, Angelo M, Bendall SC, Keene CD, Montine TJ. Mass synaptometry: High-dimensional multi parametric assay for single synapses. J Neurosci Methods. 2019 Jan 15;312:73-83. Epub 2018 Nov 20 PubMed.
- Gajera CR, Fernandez R, Montine KS, Fox EJ, Mrdjen D, Postupna NO, Keene CD, Bendall SC, Montine TJ. Mass-tag barcoding for multiplexed analysis of human synaptosomes and other anuclear events. Cytometry A. 2021 Sep;99(9):939-945. Epub 2021 Apr 5 PubMed.
- Choi J, Sullards MC, Olzmann JA, Rees HD, Weintraub ST, Bostwick DE, Gearing M, Levey AI, Chin LS, Li L. Oxidative damage of DJ-1 is linked to sporadic Parkinson and Alzheimer diseases. J Biol Chem. 2006 Apr 21;281(16):10816-24. PubMed.
- Baulac S, Lu H, Strahle J, Yang T, Goldberg MS, Shen J, Schlossmacher MG, Lemere CA, Lu Q, Xia W. Increased DJ-1 expression under oxidative stress and in Alzheimer's disease brains. Mol Neurodegener. 2009;4:12. PubMed.
- Lehrman EK, Wilton DK, Litvina EY, Welsh CA, Chang ST, Frouin A, Walker AJ, Heller MD, Umemori H, Chen C, Stevens B. CD47 Protects Synapses from Excess Microglia-Mediated Pruning during Development. Neuron. 2018 Oct 10;100(1):120-134.e6. PubMed.
- Ding X, Wang J, Huang M, Chen Z, Liu J, Zhang Q, Zhang C, Xiang Y, Zen K, Li L. Loss of microglial SIRPα promotes synaptic pruning in preclinical models of neurodegeneration. Nat Commun. 2021 Apr 1;12(1):2030. PubMed.
- Wang C, Xiong M, Gratuze M, Bao X, Shi Y, Andhey PS, Manis M, Schroeder C, Yin Z, Madore C, Butovsky O, Artyomov M, Ulrich JD, Holtzman DM. Selective removal of astrocytic APOE4 strongly protects against tau-mediated neurodegeneration and decreases synaptic phagocytosis by microglia. Neuron. 2021 May 19;109(10):1657-1674.e7. Epub 2021 Apr 7 PubMed.
- Hesse R, Hurtado ML, Jackson RJ, Eaton SL, Herrmann AG, Colom-Cadena M, Tzioras M, King D, Rose J, Tulloch J, McKenzie CA, Smith C, Henstridge CM, Lamont D, Wishart TM, Spires-Jones TL. Comparative profiling of the synaptic proteome from Alzheimer's disease patients with focus on the APOE genotype. Acta Neuropathol Commun. 2019 Dec 20;7(1):214. PubMed.
- Colom-Cadena M, Pegueroles J, Herrmann AG, Henstridge CM, Muñoz L, Querol-Vilaseca M, Martín-Paniello CS, Luque-Cabecerans J, Clarimon J, Belbin O, Núñez-Llaves R, Blesa R, Smith C, McKenzie CA, Frosch MP, Roe A, Fortea J, Andilla J, Loza-Alvarez P, Gelpi E, Hyman BT, Spires-Jones TL, Lleó A. Synaptic phosphorylated α-synuclein in dementia with Lewy bodies. Brain. 2017 Dec 1;140(12):3204-3214. PubMed.
Further Reading
Primary Papers
- Phongpreecha T, Gajera CR, Liu CC, Vijayaragavan K, Chang AL, Becker M, Fallahzadeh R, Fernandez R, Postupna N, Sherfield E, Tebaykin D, Latimer C, Shively CA, Register TC, Craft S, Montine KS, Fox EJ, Poston KL, Keene CD, Angelo M, Bendall SC, Aghaeepour N, Montine TJ. Single-synapse analyses of Alzheimer's disease implicate pathologic tau, DJ1, CD47, and ApoE. Sci Adv. 2021 Dec 17;7(51):eabk0473. Epub 2021 Dec 15 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Washington University School of Medicine
This work by Tom Montine’s group is incredible in the spatial resolution and identification of protein amounts and co-localization at the synapse in AD. It offers a new orthogonal window to peer into the molecular machinery of AD (and synapses in general) and has interesting findings of candidate proteins that may have mechanistic importance at the synapse. It’s amazing how the group developed and validated the technology to provide deep insights into AD processes—truly cutting-edge!
Emory University
This technique is useful and will certainly provide novel insight into synaptic mechanisms linked to neurodegeneration. To date, many of the proteomic analyses of postmortem brain have been performed on bulk tissue, restricting the ability to characterize cell-type-specific protein alterations. Moreover, it remains extremely challenging to efficiently capture neurons intact from brain for proteomic analysis, especially with single-cell resolution.
What is impressive about this current study is that it leverages CyTOF technology, combining principles of mass spectrometry and flow cytometry, to resolve single-synaptic events in brain. The authors have termed this technique SynTOF. Thus, analogous to single-cell or single-nuclei RNA-Seq, this allowed the authors to identify unique sub-populations of synaptosomes across disease states.
This included synaptosomes with increased hippocampal pathologic tau in AD and reduced levels of the dopamine transporters in LBD. Interestingly, they showed some hippocampal synapses with increased levels of the CD47 in AD, which is a marker that would be predicted to protect the synapse from excessive microglial pruning and degradation.
Limitations of the approach include dependence on high-quality antibodies and that despite creating more than 100 synaptosome preparations, a relatively small number were suitable for SynTOF analyses. Better cryopreservation techniques could potentially be key to advancing this exciting approach.
The University of Queensland
Using a mass-cytometry–based method, synaptometry by time of flight (SynTOF), this study focuses on the synapse to uncover what causes AD. I generally like this elegant approach, but believe it adds an additional variable compared to more classical mass-spec approaches.
The authors screened 166 antibodies to arrive at 38 with high specificity. Just as the utility of a model depends on the validity of the underlying assumptions, SynTOF used here depends on the quality of the antibodies employed. It seems to me that, ideally, one would use more than one antibody for a given target.
I did like the fact that two AD-resilient cases were analyzed among the nine ADNC cases.
I am convinced that this methodology will be widely adopted.
University of Edinburgh
This interesting study by Montine and colleagues examines the composition of synapses using mass cytometry. It is surprising that they do not observe Aβ in human synapses from AD patient brain, because we and others have observed this using multiple methods, including high-resolution imaging and biochemical enrichment of synaptic fractions (see, for example, Koffie et al., 2012; Jackson et al., 2019; Perez-Nievas et al., 2013). Perhaps the Aβ antibodies used for their assay do not detect the oligomeric Aβ that we have observed in human synapses.
The APOE data are also not consistent with some of our previous work using array tomography, where we saw no increase in the proportion of synapses in AD brain containing APOE, although we cannot rule out that those synapses that did contain APOE had higher levels of the apolipoprotein in our study (Koffie et al., 2012). It would be good to see how the current results differ based on APOE genotype of the donors.
The tau synapse data are consistent with our observations, both from proteomics and high-resolution imaging (Hesse et al., 2019; Zhou et al., 2017; Pickett et al., 2019). The CD47 data are also consistent with our data using unbiased proteomics mass-spec analysis of human synapses (Hesse et al., 2019).
It is super interesting to see how things replicate (or don't) in studies by other groups. I'm very glad to see the growing interest in synaptic composition in AD!
References:
Hesse R, Hurtado ML, Jackson RJ, Eaton SL, Herrmann AG, Colom-Cadena M, Tzioras M, King D, Rose J, Tulloch J, McKenzie CA, Smith C, Henstridge CM, Lamont D, Wishart TM, Spires-Jones TL. Comparative profiling of the synaptic proteome from Alzheimer's disease patients with focus on the APOE genotype. Acta Neuropathol Commun. 2019 Dec 20;7(1):214. PubMed.
Jackson RJ, Rose J, Tulloch J, Henstridge C, Smith C, Spires-Jones TL. Clusterin accumulates in synapses in Alzheimer's disease and is increased in apolipoprotein E4 carriers. Brain Commun. 2019;1(1):fcz003. Epub 2019 Jun 24 PubMed.
Koffie RM, Hashimoto T, Tai HC, Kay KR, Serrano-Pozo A, Joyner D, Hou S, Kopeikina KJ, Frosch MP, Lee VM, Holtzman DM, Hyman BT, Spires-Jones TL. Apolipoprotein E4 effects in Alzheimer's disease are mediated by synaptotoxic oligomeric amyloid-β. Brain. 2012 Jul;135(Pt 7):2155-68. PubMed.
Perez-Nievas BG, Stein TD, Tai HC, Dols-Icardo O, Scotton TC, Barroeta-Espar I, Fernandez-Carballo L, de Munain EL, Perez J, Marquie M, Serrano-Pozo A, Frosch MP, Lowe V, Parisi JE, Petersen RC, Ikonomovic MD, López OL, Klunk W, Hyman BT, Gómez-Isla T. Dissecting phenotypic traits linked to human resilience to Alzheimer's pathology. Brain. 2013 Aug;136(Pt 8):2510-26. PubMed.
Pickett EK, Herrmann AG, McQueen J, Abt K, Dando O, Tulloch J, Jain P, Dunnett S, Sohrabi S, Fjeldstad MP, Calkin W, Murison L, Jackson RJ, Tzioras M, Stevenson A, d'Orange M, Hooley M, Davies C, Colom-Cadena M, Anton-Fernandez A, King D, Oren I, Rose J, McKenzie CA, Allison E, Smith C, Hardt O, Henstridge CM, Hardingham GE, Spires-Jones TL. Amyloid Beta and Tau Cooperate to Cause Reversible Behavioral and Transcriptional Deficits in a Model of Alzheimer's Disease. Cell Rep. 2019 Dec 10;29(11):3592-3604.e5. PubMed.
Zhou L, McInnes J, Wierda K, Holt M, Herrmann AG, Jackson RJ, Wang YC, Swerts J, Beyens J, Miskiewicz K, Vilain S, Dewachter I, Moechars D, De Strooper B, Spires-Jones TL, De Wit J, Verstreken P. Tau association with synaptic vesicles causes presynaptic dysfunction. Nat Commun. 2017 May 11;8:15295. PubMed.
Northwestern University Feinberg School of Medicine
This is an interesting technology with the potential for deep interrogation of protein content in synapses and how they change with age or disease. It would be interesting to see if the technology could be adapted to interrogate other parts of the neuron, such as axons, dendrites, or organelles, including mitochondria, lysosomes, and the nucleus.
I don’t see the results as pointing to a shortcoming of the mouse models. Postmortem human AD brain represents end-stage disease, consisting of burned-out plaques and tangles—lesions that are tombstones. Therefore, it is not surprising that the human AD synapses did not contain Aβ, because they were end-stage, highly degenerated, and dysfunctional.
In contrast, the AD mouse models represent early, preclinical AD, wherein the pathogenic processes are active and progressing, but are not burned out, as is the case in postmortem human AD. Hence, the PS/APP mouse synapses were actively producing Aβ.
I think this technology will be very informative for earlier-stage human neurodegenerative diseases, but we should be cautious interpreting the results from end-stage AD or other neurodegenerations.
Ludwig-Maximilians-Universität Munich
This is certainly an exceptional study on synaptosomes prepared from fresh human brain. Most studies on “synaptosomes” from human tissue are done with frozen material and that does not lead to “real” synaptosomes. I am indeed fascinated by the data obtained in control patients.
However, as a neuropathologist, I have difficulty judging the results obtained in humans with Aβ or/and α-synuclein pathology when the ApoE genotype is not given. LBD cases of old age without significant Aβ pathology are very rare—if it occurs these are often PD cases without any ApoE4 allele. So, I assume that the ApoE genotypes are significantly different between the groups compared in this study. But the authors could tell us. To me the statement comparing “pure AD” with “LBD” in the abstract is problematic since Aβ pathology is most often found in both.
In nearly all mouse amyloid models, the synaptic pathology is restricted to the area close to amyloid plaques, but in humans with AD there is severe tau pathology and synapse loss distant to plaques (Peters et al., 2018). So, I would not expect similar results when comparing synaptosomes from mouse amyloid models and humans with AD-related pathology. The amyloid models are only models for some aspects of AD related to Aβ accumulation—indeed, not for those that are attributed to p-tau accumulation, for example.
References:
Peters F, Salihoglu H, Rodrigues E, Herzog E, Blume T, Filser S, Dorostkar M, Shimshek DR, Brose N, Neumann U, Herms J. BACE1 inhibition more effectively suppresses initiation than progression of β-amyloid pathology. Acta Neuropathol. 2018 May;135(5):695-710. Epub 2018 Jan 11 PubMed.
National Institute on Aging
This technique is very interesting and could be more widely applied across neurodegenerative diseases. In particular, it would be really interesting to see which changes in disease are specific to AD, and which are due to damaged synapses reacting to disease more generally. For example, I’d like to see if DJ-1 levels are lower in synapses in dopamine neurons in Parkinson’s early in disease.
To this point, it is probably going to be really tough to work in studies of early disease in people, i.e., before frank pathology has set in, so I wonder if one interpretation of discrepancies between the human and mouse data is that the latter are due to the very earliest of events.
University of California, San Diego
I think this method has potentially important applications.
However, it is important to note that the analyses in this study were limited to presynaptic structures. Most synaptic studies in AD models that I’m aware of, but then I’m likely biased by my area of expertise, have observed postsynaptic changes, for example in synaptic glutamate receptor number. Other types of studies on human AD brain samples have seen reductions in PSD-95, a postsynaptic protein that is important in synaptic function. As a side note, elevated PSD-95 can protect synapses from Aβ (Dore et al., 2021).
It may be potentially more relevant to AD to analyze postsynaptic protein composition with this type of method. Unfortunately, the synaptosome preparation used in this study is largely limited to presynaptic proteins. I don’t know of a biochemical preparation akin to synaptosomes that contains primarily postsynaptic proteins.
References:
Dore K, Carrico Z, Alfonso S, Marino M, Koymans K, Kessels HW, Malinow R. PSD-95 protects synapses from β-amyloid. Cell Rep. 2021 Jun 1;35(9):109194. PubMed.
The University of Tokyo
This is certainly a tour de force of proteomic analyses. In combination with machine learning, the authors found several differences in the protein expressions of key proteins, such as CD47, DJ-1, and ApoE in AD brains. They also implied that, for the first time, ApoE might be an important factor for resilience against AD pathology.
Further comparisons might reveal the neurodegenerative process at a molecular level in situ.
Make a Comment
To make a comment you must login or register.