Does Cognition Change With the Seasons?
Quick Links
For everything there is a season—perhaps even cognition? A September 4 paper in PLoS Medicine reports that people tested on neuropsychological tests in the summer and fall outperformed people tested in the winter and spring. The ebb and flow of scores tracked with levels of Aβ in people’s cerebrospinal fluid, as well as with expression of certain sets of genes in their brains. Importantly, the study was not longitudinal, but cross-sectional, i.e., different sets of people took the test in the different seasons. Still, the findings at least hint at a potential source of noise in clinical trials, said lead author Andrew Lim, University of Toronto, who conducted the study with senior author Philip De Jager, Columbia University, New York.
- People tested in the summer and fall performed better on neuropsychological tests than those quizzed in the winter/spring.
- A diagnosis of MCI or Alzheimer’s is more common in colder months.
- Seasonal scores fluctuate with changes in gene expression and CSF Aβ.
“This is a provocative exploratory study,” said Lon Schneider, University of Southern California, Los Angeles, who was not involved in the work. The magnitude of the seasonal differences the authors report are as big as the clinical effect researchers look for in clinical trials. “If not planned for in trial design, this potential effect could easily confound outcomes of clinical trials in either the positive or negative direction, or wash out the potential to see change,” Schneider said.
“These findings are very interesting and important,” wrote Erik Musiek, Washington University School of Medicine, St. Louis, to Alzforum (see full comment below). “They could explain some year-to-year variability in cognitive performance in patients and research participants.”

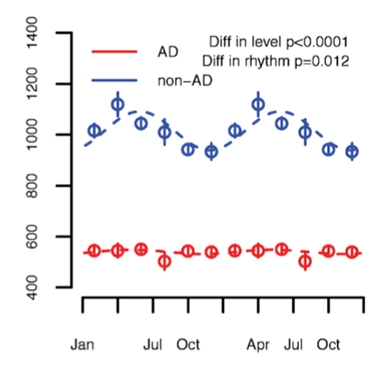
Seasonal change.
On average, global cognitive scores are higher in the summer/fall than in the winter/spring. Circles represent groups of people assessed within two months of each other. [Courtesy of Lim et al., 2018.]
Seasonal changes in cognition are far from a new finding. They have been reported previously in young adults in northern latitudes (Brennan et al., 1999; Meyer et al., 2016). However, when Lim and colleagues detected periodic transcriptional and epigenetic changes in the brains of older adults, they began to wonder if cognition fluctuated seasonally in older people, as well (Lim et al., 2017). “We wanted to know whether we would see similar rhythms in a population of older individuals who are at risk for cognitive impairment,” Lim told Alzforum. “Such variations may be clinically important.”
The scientists analyzed data collected from five different longitudinal cohorts. From the Rush Memory and Aging Project (MAP), the Religious Orders Study (ROS), and the Minority Aging Research Study (MARS), which enrolls African-American participants, the researchers correlated baseline neuropsychological evaluations of 2,761 volunteers with the season when that data was collected. The participants were cognitively normal when they enrolled. Any who died were autopsied and the expression of RNA in their brains measured by RNASeq. From a fourth cohort, the Centre de Neurologie Cognitive (CNC) study at Lariboisière Hospital in Paris, the authors obtained cerebrospinal fluid (CSF) biomarker data on 321 participants both with and without Alzheimer’s disease. Lastly, from the Sunnybrook Dementia Study (SDS) in Toronto, the researchers incorporated cognitive data from 271 patients with clinical dementia.
On average, people from the ROS, MAP, and MARS studies who were evaluated in the summer or fall did better on neuropsychological tests than people tested in the winter and early spring (see image above). Relative to the mean score for the entire group across all seasons, a composite measure of global cognition varied from summer peak to winter trough by 0.2 to 0.3 standard deviations. That roughly equates to a 4.8-year difference in cognitive aging, the authors wrote. The greatest difference emerged in tests of working memory and speed of perception. It held up when depressive symptoms at the time, amount of sleep over the preceding month, and physical activity in the previous two weeks were taken into account. While smaller, a seasonal oscillation in cognition was also apparent among people who had AD.
This latter fluctuation seemed to have a practical effect on diagnosis. People in the ROS, MAP, or MARS studies who were evaluated in the winter or spring were 24 percent more likely to be diagnosed with mild cognitive impairment or AD than those evaluated in the summer.
What could drive cognition to rise and fall with the seasons? The authors turned to biomarkers. In the Lariboisière cohort, CSF Aβ42 levels, but not tau or phosphorylated tau, changed with the seasons in people without AD, peaking at the end of June (see image below). CSF Aβ42 also varied over the year in AD patients, though by a smaller amount.
CSF Markers.
Aβ42 levels change with the season in people without AD, peaking in late June. People with AD show much subtler changes. [Courtesy of Lim et al., 2018.]
Seasonal changes in gene expression, too, tracked with the cognition swings. Sampling blocks of postmortem tissue from the dorsolateral prefrontal cortex, a region involved in working memory, Lim and colleagues found rhythmic variation in clusters of correlated genes among 507 donors. Four such gene modules varied with cognition—two rose and fell along with it, and two fluctuated in the opposite direction. One of the latter modules was enriched in genes important for modifying chromatin and controlling the cell cycle.
The authors were careful to note that in these observational studies, people came for cognitive testing once a year at about the same time of year, so there were no seasonal data within a given participant. “The most we can say is that as a group, people assessed in late summer and early fall have a substantially better cognitive performance than people assessed in the winter or early spring,” said Lim.
Li-Huei Tsai from MIT, who was not involved in this work, said that future studies would be needed to confirm these findings. “If we want to make scientific conclusions, we’ll have to follow the same individuals through the seasons,” Tsai said. She found it interesting that CSF Aβ42 levels fluctuate by season, since they are already known to fluctuate throughout the day (Bateman et al., 2007).
Tsai also was intrigued that time of year a study reads out could affect its outcome. “It adds to the complexity of the disease,” she said. She agreed with the authors that understanding the mechanisms behind this seasonal fluctuation could help identify new targets for interventions.
Musiek noted that the questionnaires used in this study may not have been sensitive enough to pick up on subtle differences in mood between seasons. “Mood, motivation, and anxiety are all things that might change seasonally and influence test performance,” he wrote to Alzforum. Yue Leng, University of California, San Francisco, added to that list. “Hormone levels, temperature, humidity, sleep timings could all be different in summer versus winter,” she said. Musiek noted that regardless of the underlying mechanisms, this variation is important to consider from a clinical study/clinical trial standpoint.
Because the studies’ participants were all at northern latitudes, it would be interesting to relate cognition to season in the southern hemisphere and in people living near the equator, said Lim.
The authors plan to study possible environmental factors behind the seasonal differences in cognition and whether those differences affect people’s daily lives. If ambient light, physical activity, or social interactions are responsible, those could be modified to improve cognition year-round, they wrote.
For her part, Suzanne Hendrix, Pentara Corporation, Salt Lake City, Utah, has seen a seasonal effect on symptoms in Parkinson’s. In PD patients, scores on the Unified Parkinson's Disease Rating Scale, which includes cognitive items, were better in the summer than in the winter. Accounting for that fluctuation reduced variability in the data, giving her more power to detect a treatment difference. Such a strategy could work in AD trials as well. “The effect sizes they are seeing here are quite big,” Hendrix told Alzforum. “[Season] could be interfering with our ability to see treatment effects.”—Gwyneth Dickey Zakaib
References
Paper Citations
- Brennen T, Martinussen M, Hansen BO, Hjemdal O. Arctic cognition: a study of cognitive performance in summer and winter at 69 degrees N. Appl Cogn Psychol. 1999 Dec;13(6):561-80. PubMed.
- Meyer C, Muto V, Jaspar M, Kussé C, Lambot E, Chellappa SL, Degueldre C, Balteau E, Luxen A, Middleton B, Archer SN, Collette F, Dijk DJ, Phillips C, Maquet P, Vandewalle G. Seasonality in human cognitive brain responses. Proc Natl Acad Sci U S A. 2016 Mar 15;113(11):3066-71. Epub 2016 Feb 8 PubMed.
- Lim AS, Klein HU, Yu L, Chibnik LB, Ali S, Xu J, Bennett DA, De Jager PL. Diurnal and seasonal molecular rhythms in human neocortex and their relation to Alzheimer's disease. Nat Commun. 2017 Apr 3;8:14931. PubMed.
- Bateman RJ, Wen G, Morris JC, Holtzman DM. Fluctuations of CSF amyloid-beta levels: implications for a diagnostic and therapeutic biomarker. Neurology. 2007 Feb 27;68(9):666-9. PubMed.
Further Reading
Primary Papers
- Lim AS, Gaiteri C, Yu L, Sohail S, Swardfager W, Tasaki S, Schneider JA, Paquet C, Stuss DT, Masellis M, Black SE, Hugon J, Buchman AS, Barnes LL, Bennett DA, De Jager PL. Seasonal plasticity of cognition and related biological measures in adults with and without Alzheimer disease: Analysis of multiple cohorts. PLoS Med. 2018 Sep;15(9):e1002647. Epub 2018 Sep 4 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
The Florey Institute for Neuroscience and Mental Health
This is a fascinating paper showing seasonal differences in cognition and related biological measures. The authors show that cognitive performance peaks around the time of the fall equinox. The impact of seasonal variation on cognition is large, equivalent to ~four years of normal brain aging. The authors lend plausibility to their findings by reproducing the association in multiple cohorts. They also demonstrate that findings are clinically important by showing that participants had almost 30 percent higher odds of clinical cognitive impairment or dementia in winter and spring compared with summer and fall. Lastly, the authors looked at biological variables and showed that CSF A42 levels peaked during the summer and that season was also tied to the brain expression of gene modules related to cognition.
The factors contributing to these findings are intriguing and require further investigation. In this study, the authors adjusted for age, sex, years of education, depressive symptoms, hours of sleep and physical activity, and serum TSH. However, as noted by the authors, other aspects of lifestyle (i.e., diet), sleep (circadian alignment and sleep quality) and mood may potentially drive seasonal differences in cognition. Seasonal differences in hormones and vitamin D may also contribute.
Not all countries experience such distinct seasons. Participants from this study were mostly from temperate regions of the northern hemisphere. It would be interesting to investigate seasonal differences in cognition and related biological variables in regions where temperature and sunlight are more stable throughout the year. For example, the opposite findings might be expected in the southern hemisphere, with cognition peaking in February. Also, perhaps people in countries close to the equator may show no seasonal differences.
One limitation of the study is that it compared between people, rather than within people. Understanding individual trajectories of cognitive function across the year may also be informative.
These results may have diagnostic implications. Neuropsychologists and physicians should already be cognizant of the fact that a single neuropsychological assessment can underestimate performance; seasonality may be one contributor that needs to be considered. Whereas dementia diagnosis is not based solely on cognitive test data, mild cognitive impairment is often diagnosed based on comparing neuropsychological scores to a normative sample. Many persons diagnosed with MCI may revert back to normal. Repeated cognitive assessments across the year may provide more robust estimates of cognition and reduce the rate of false positive classifications. Pending further replication of these findings in diverse geographical areas, seasonal cognitive test norms could also be considered.
Washington University School of Medicine
This paper builds on work from the same lab showing seasonal variation in brain gene expression, and the data are in keeping with other studies linking seasonality to cognition (Meyer et al., 2016). These findings are very interesting and important, as they could explain some year-to-year variability in cognitive performance (and CSF Aβ levels) in patients and research participants. Much as time of day can influence these parameters, this paper would suggest that time of year does as well, and that memory clinics, research studies, and clinical trials might investigate this phenomenon further and, if needed, consider some type of adjustment.
Certainly, longitudinal studies would be very helpful in evaluating this further. One concern I have is that the specific questionnaires used to detect depression in these studies may lack sensitivity to detect more subtle changes in mood that might impact cognitive test performance. Seasonal variation in other hormones besides TSH, such as cortisol, or in autonomic function, could contribute.
While the molecular machinery driving circadian timing in the body is now understood, it is unknown if a seasonal clock exists, and if so, what it is or how it works. It is simplest to assume that these changes represent responses to the changing environment, but it is possible that an undiscovered seasonal clock regulates gene expression. Seasonal change in many aspects of peripheral metabolism have been demonstrated, and perhaps the brain is responding to those. The most obvious potential mechanism is that changes in the amount and timing of light exposure influence the circadian clock, which can directly regulate gene transcription. There are clear effects of photoperiod on mood (seasonal affective disorder), and it is well established that the circadian clock can influence learning and memory systems. However, many variables change seasonally, so there are many potential explanations.
References:
Meyer C, Muto V, Jaspar M, Kussé C, Lambot E, Chellappa SL, Degueldre C, Balteau E, Luxen A, Middleton B, Archer SN, Collette F, Dijk DJ, Phillips C, Maquet P, Vandewalle G. Seasonality in human cognitive brain responses. Proc Natl Acad Sci U S A. 2016 Mar 15;113(11):3066-71. Epub 2016 Feb 8 PubMed.
Make a Comment
To make a comment you must login or register.