Dearth of Water Channels a Sign of ‘Glymphatic’ Breakdown in Alzheimer’s?
Quick Links
Amyloid builds up in the brains of people with Alzheimer’s disease, and in the more common, sporadic form of AD, inefficient clearance of Aβ may be the main culprit. A study published in the November 28 issue of JAMA Neurology lends credence to this idea. Researchers led by Jeffrey Iliff at the Oregon Health & Science University, Portland, report that a water channel called aquaporin 4 (Aqp4) goes missing from its normal site surrounding blood vessels in AD, suggesting that one of the brain’s clearance systems, the “glymphatic” pathway, may be compromised.
A brain-wide glymphatic pathway was defined in 2012 by Maiken Nedergaard of the University of Rochester Medical Center, New York, and her colleagues, including Iliff. The pathway allows interstitial fluid to circulate quickly and deeply within the brain, aided by the flow of water through Aqp4 channels. Aqp4 is strategically positioned on the end-feet of astrocytes that form a space around blood vessels through which the fluid flows (Iliff et al., 2012). “Aqp4 creates a preferential pathway, a low-resistance route for water transport,” explained Iliff. The flow is thought to start along the outside of arteries and arterioles, move through the brain tissue and then out along veins and venules, whisking away waste particles lodged between cells, including Aβ.
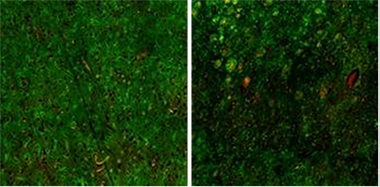
Flow-stopper.
Aquaporin-4 water channels (green) normally occur on perivascular sites in young brains (left) but much less so in Alzheimer’s brains (right). Large red spots are Aβ plaques. [Image courtesy of Jeffrey Iliff.]
Suspecting that aging might take a toll on the glymphatic pathway, Iliff and co-workers examined its function in mice. Previously, they had reported an age-dependent loss of perivascular Aqp4 that correlated with impaired clearance of Aβ injected into the brains of otherwise normal mice (Kress et al., 2014). The findings were consistent with earlier studies from Carol Colton at Duke University in Durham, North Carolina, who found less Aqp4 in astrocytic end feet in four mouse models of cerebral amyloid angiopathy than in wild-type controls. (Wilcock et al., 2009). The findings were intriguing because they suggested a breakdown of the glymphatic pathway that could play a role in AD, said Iliff.
Would this hold true in people? Colton’s 2009 study hinted it might since she found a negative correlation between AD severity and postmortem perivascular Aqp4 in cerebral cortex tissue. Others have reported higher global Aqp4 expression in AD compared to healthy controls (Moftakhar et al., 2010) or that Aqp4 levels vary around plaques (Hoshi et al., 2012).
To expand on this, Iliff and colleagues used immunofluorescence and western blots to track Aqp4 expression levels and localization, and quantitatively assess how they correlated with age, amyloid plaque density, and AD pathology. Analyzing postmortem tissues from the frontal cortices of 21 people with AD and 58 healthy volunteers between 33 and 105 years old, the researchers found that older people and those with AD had a moderate increase in total Aqp4 expression as assessed by immunostaining. Western blots showed no difference in Aqp4 expression between the groups, but this may be due to differences between the areas of tissue sampled with each technique, suggested the authors.
More strikingly, however, the researchers found drastic differences in the location of Aqp4 among young and old brains and healthy and AD brains. Aqp4 uniformly distributed from the cortical surface to the subcortical white matter boundary in normal people younger than 60. In people 60-85 and in people with AD, Aqp4 was intensely expressed only in a sparse population of cortical astrocytes. Large patches of tissue showed faint Aqp4 staining, particularly in the deep cortical layers. At higher magnification, the researchers found that perivascular Aqp4 in particular was strongly reduced in AD brains, and, though to a lesser extent, in aged brains. Loss of perivascular Aqp4 in AD tissue tracked with both Aβ plaque density and Braak staging. Also, in AD brains, the researchers saw bright foci of Aqp4 associated with Aβ plaques, although, as in aged individuals, Aqp4 staining across most of the deep cortical expanse was lower than normal (see image above).
This corroborates the rodent data and supports further exploration of the role of the glymphatic system and aquaporin in AD pathology, said Iliff. The study also offered some clues about people who remain sharp far into old age. Remarkably, when the researchers examined brain tissue obtained from such people older than 85, they found Aqp4 staining patterns that were much more like those of healthy, young people than those of the 65- to 80-year-olds or people with AD. “We might be seeing a survivor effect,” said Iliff. This Aqp4 preservation could be protective, but it could also be an epiphenomenon.
What this loss of perivascular Aqp4 in AD means remains uncertain. “It’s a chicken-and-egg question,” noted Costantino Iadecola at the Weill Cornell Medical College in New York. “What comes first: Is it the aquaporin loss that leads to reduced Aβ clearance? Or is the reduced Aβ clearance resulting in loss of aquaporin? That’s really the million-dollar question.”
Iliff suspects there’s a little of both chicken and egg. There could be a nasty feed-forward cycle, where loss of perivascular Aqp4 causes a buildup of Aβ, which in turn causes more Aqp4 to be lost. However, he noted that the drop in perivascular Aqp4 occurred in some people without visible plaques, suggesting it may happen early in disease. It could be that vascular dysfunction sets the stage for the pathological cycle. That dovetails with other studies placing low blood flow due to atherosclerosis or increased vascular stiffness, or low-level breakdown in the blood-brain barrier, into the cascade that leads to AD pathology.
Others cautioned that much remains unknown about the basics of the glymphatic system. That the equilibration of CSF with interstitial fluid in the brain parenchyma depends on the presence of Aqp4 in astrocyte end-feet has been well established, noted Roy Weller, University of Southampton, England, in an email to Alzforum (see Rennels 1985; Iliff et al., 2012). “What is not certain is the perivenous pathway that this group has suggested as the route for elimination of CSF and tracers that have entered the brain,” he wrote. As a next step, Weller suggested measuring Aqp4 around different blood vessel types—arteries, capillaries, and veins—to determine which are most affected by aging and AD pathology.
Colton suggested looking beyond Aqp4 to see in what other ways astrocytes are altered and why Aqp4 vanishes from their end-feet. She had found certain potassium channels, as well as dystrophin, a protein that anchors channels to cell membranes, to be reduced at perivascular sites. Perhaps the loss of dystrophin sets several membrane channels loose, including Aqp4, so that they are no longer tethered to their normal sites of action, she said. Iliff plans to explore the molecular underpinnings of the change in Aqp4 localization and to search for upstream changes that might make targets for therapeutic intervention.
“The most important step will be to measure this [Aqp4] biology in living, breathing humans,” said Iliff. He wants to use MRI and PET to measure the dynamics of contrast agents injected into the brain and to develop ligands to track particular molecules. A PET ligand for Aqp4 is already under development (Nakamura et al., 2011).—Marina Chicurel
Marina Chicurel is a science writer based in Santa Cruz, California.
References
News Citations
Paper Citations
- Kress BT, Iliff JJ, Xia M, Wang M, Wei HS, Zeppenfeld D, Xie L, Kang H, Xu Q, Liew JA, Plog BA, Ding F, Deane R, Nedergaard M. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. 2014 Dec;76(6):845-61. Epub 2014 Sep 26 PubMed.
- Wilcock DM, Vitek MP, Colton CA. Vascular amyloid alters astrocytic water and potassium channels in mouse models and humans with Alzheimer's disease. Neuroscience. 2009 Mar 31;159(3):1055-69. Epub 2009 Jan 19 PubMed.
- Moftakhar P, Lynch MD, Pomakian JL, Vinters HV. Aquaporin expression in the brains of patients with or without cerebral amyloid angiopathy. J Neuropathol Exp Neurol. 2010 Dec;69(12):1201-9. PubMed.
- Hoshi A, Yamamoto T, Shimizu K, Ugawa Y, Nishizawa M, Takahashi H, Kakita A. Characteristics of aquaporin expression surrounding senile plaques and cerebral amyloid angiopathy in Alzheimer disease. J Neuropathol Exp Neurol. 2012 Aug;71(8):750-9. PubMed.
- Rennels ML, Gregory TF, Blaumanis OR, Fujimoto K, Grady PA. Evidence for a 'paravascular' fluid circulation in the mammalian central nervous system, provided by the rapid distribution of tracer protein throughout the brain from the subarachnoid space. Brain Res. 1985 Feb 4;326(1):47-63. PubMed.
- Nakamura Y, Suzuki Y, Tsujita M, Huber VJ, Yamada K, Nakada T. Development of a Novel Ligand, [C]TGN-020, for Aquaporin 4 Positron Emission Tomography Imaging. ACS Chem Neurosci. 2011 Oct 19;2(10):568-571. Epub 2011 Jun 27 PubMed.
Further Reading
No Available Further Reading
Primary Papers
- Zeppenfeld DM, Simon M, Haswell JD, D'Abreo D, Murchison C, Quinn JF, Grafe MR, Woltjer RL, Kaye J, Iliff JJ. Association of Perivascular Localization of Aquaporin-4 With Cognition and Alzheimer Disease in Aging Brains. JAMA Neurol. 2017 Jan 1;74(1):91-99. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
University of South Alabama
University of Southern California, Keck School of Medicine
University of Southern California
Aquaporin-4 (Aqp4) is a major water channel in the human brain, located mainly in the astrocytic end-feet around cerebral blood vessels. Aqp4 plays a number of physiological roles in brain, including regulation of extracellular space volume, and ion and water homeostasis (Nagelhus and Ottersen, 2013). Here, Zeppenfeld et al. sought to determine whether Aqp4 expression is changed in normal aging and Alzheimer’s disease. They performed immunohistochemistry and western blot analysis in postmortem frontal cortical brain tissue from cognitively normal young, cognitively normal old, and AD patients. Using immunofluorescence staining, the authors found that total Aqp4 immunoreactivity levels are increased in AD compared to cognitively normal young and old subjects. Interestingly, perivascular (PV) Aqp4 was decreased in AD compared to age-matched controls. Their representative images of aged Aqp4 shows a strikingly different expression pattern compared to young, eldest, and AD subjects.
It would be intriguing to find out why Aqp4 distribution would change so drastically in aged subjects and then revert back to look like the young subject in eldest and AD subjects. A previous study, however, did not show this altered distribution in aged control subjects (Pérez et al., 2007). Upon measuring Aqp4 levels by western blot analysis, Zeppenfeld et al. found no significant changes among all groups in total Aqp4. But they did find that the ratio between Aqp4 isoforms (full-length Aqp4-M1 and truncated Aqp4-M23) is changed.
Unfortunately, it appears that the authors have mislabeled Aqp4-M1 and Aqp4-M23 in their representative blot in eFigure 3; thus currently their results reflect this mislabeling. The authors state that Aqp4-M1 significantly declined in aged cortex, but their representative blot actually shows that Aqp4-M1 significantly increased in aged and AD cortex. It would be intriguing to find out the functional significance of these findings that is not discussed in the paper. Furthermore, the importance of this altered ratio of Aqp4 isoforms during aging and AD remains to be determined. Altogether, the authors suggest that loss of perivascular expression of Aqp4 in the aging brain may affect clearance of Aβ from brain interstitial fluid by the glymphatic system.
Several studies have previously investigated Aqp4 level changes in human AD brain tissue (Hoshi et al., 2012; Moftakhar et al., 2010; Pérez et al., 2007; Potokar et al., 2016; Wilcock et al., 2009). Pérez et al. performed quantitative real-time RT-PCR and western blot of total brain homogenates of frontal cortex from control and AD subjects and found no significant difference in Aqp4 expression between groups (Pérez et al., 2007), as similarly found by Zeppenfeld et al. Wilcock et al. performed quantitative RT-PCR and immunohistochemistry on medial temporal lobe cortical tissue from control subjects and AD subjects with mild, moderate, or severe cerebral amyloid angiopathy (CAA) (Wilcock et al., 2009). They found that there were no major changes in Aqp4 mRNA or expression levels along blood vessels from AD subjects with mild AD (Wilcock et al., 2009). However, Aqp4 mRNA and expression levels were reduced with moderate and severe CAA, and less Aqp4 was observed along blood vessels (Wilcock et al., 2009). Hoshi et al. performed Aqp4 and Aβ immunohistochemistry on temporal lobe tissue from control, sporadic AD, and familial AD subjects and found that Aqp4 is variably distributed near Aβ40 and Aβ42 senile plaques (Hoshi et al., 2012). Moftakhar et al. investigated Aqp4 using immunohistochemistry in frontal, temporal, and occipital cortex to assess expression of Aqp4 levels in control and AD subjects with varying degrees of CAA (Moftakhar et al., 2010). They found that Aqp4 expression was enhanced in AD and was prominent at the CSF fluid and brain interfaces including subpial, subependymal, pericapillary, and periarteriolar spaces (Moftakhar et al., 2010).
Although the jury is still out, the “glymphatic system” has attracted a lot of interest and attention in the field. It has revived the importance of the perivascular fluid flow hypothesis in overall brain homeostasis, with important potential implications to disease states. The term “glymphatic system” was originally coined to better reflect the concept that the brain does not have a proper lymphatic system. However, recent work from other groups has convincingly demonstrated the existence of the lymphatic system in the brain and connections of brain interstitial fluid (ISF) and cerebrospinal fluid (CSF) pathways with lymphatic meningeal vessels and the lymph nodes in the neck (Aspelund et al., 2015; Louveau et al., 2015).
These recent discoveries raise an important question. What, then, would be the postulated role of the glymphatic system if a normal lymphatic system already exists in the brain? Of note, the perivascular drainage pathway connected to brain lymphatic system renamed later as a “glymphatic system” was discovered in the late 1970s and early 1980s, when astrocyte regulation of the ISF flow via this pathway had not been known.
The question in the field remains, however, whether the direction of the ISF flow in the brain is from brain ISF to CSF to serve for clearance of brain metabolic waste products such as Alzheimer’s Aβ, as claimed by Carare-Weller’s hypothesis and several earlier studies from Bradbury, Davson, Segal, and other groups, or from CSF recycling back to brain, as claimed by the authors of the glymphatic system hypothesis. It is important to remember that the majority of Aβ is cleared from brain under physiological conditions by transvascular clearance across the blood-brain barrier (Tarasoff-Conway et al., 2015).
Future studies should investigate what happens to the brain lymphatic system in Alzheimer’s disease and other neurodegenerative diseases, and interactions with perivascular clearance, and how this is influenced by volume changes in astrocytes mediated by Aqp4 that is central to the so-called glymphatic regulation of flow.
References:
Aspelund A, Antila S, Proulx ST, Karlsen TV, Karaman S, Detmar M, Wiig H, Alitalo K. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J Exp Med. 2015 Jun 29;212(7):991-9. Epub 2015 Jun 15 PubMed.
Hoshi A, Yamamoto T, Shimizu K, Ugawa Y, Nishizawa M, Takahashi H, Kakita A. Characteristics of aquaporin expression surrounding senile plaques and cerebral amyloid angiopathy in Alzheimer disease. J Neuropathol Exp Neurol. 2012 Aug;71(8):750-9. PubMed.
Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, Derecki NC, Castle D, Mandell JW, Lee KS, Harris TH, Kipnis J. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015 Jul 16;523(7560):337-41. Epub 2015 Jun 1 PubMed.
Moftakhar P, Lynch MD, Pomakian JL, Vinters HV. Aquaporin expression in the brains of patients with or without cerebral amyloid angiopathy. J Neuropathol Exp Neurol. 2010 Dec;69(12):1201-9. PubMed.
Nagelhus EA, Ottersen OP. Physiological roles of aquaporin-4 in brain. Physiol Rev. 2013 Oct;93(4):1543-62. PubMed.
Pérez E, Barrachina M, Rodríguez A, Torrejón-Escribano B, Boada M, Hernández I, Sánchez M, Ferrer I. Aquaporin expression in the cerebral cortex is increased at early stages of Alzheimer disease. Brain Res. 2007 Jan 12;1128(1):164-74. PubMed.
Potokar M, Jorgačevski J, Zorec R. Astrocyte Aquaporin Dynamics in Health and Disease. Int J Mol Sci. 2016 Jul 13;17(7) PubMed.
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, Axel L, Rusinek H, Nicholson C, Zlokovic BV, Frangione B, Blennow K, Ménard J, Zetterberg H, Wisniewski T, de Leon MJ. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015 Aug;11(8):457-70. Epub 2015 Jul 21 PubMed.
Wilcock DM, Vitek MP, Colton CA. Vascular amyloid alters astrocytic water and potassium channels in mouse models and humans with Alzheimer's disease. Neuroscience. 2009 Mar 31;159(3):1055-69. Epub 2009 Jan 19 PubMed.
Nanjing Medical University
Age-associated accumulation of Aβ peptides and hyperphosphorylated tau is a central event in the pathogenesis of Alzheimer’s disease. The misaggregation of these toxic proteins has been hypothesized to result from an imbalance between their production and clearance (Ross et al., 2004). Thus, it is critical to understand how toxic metabolites are cleared from the brain, which might contribute to developing promising strategies for delaying or even halting AD onset (Tarasoff-Conway et al., 2015).
Findings from the past few years suggest that a brain-wide perivascular pathway, termed the glymphatic system, contributes to a larger portion of clearance of interstitial solutes, including Aβ and tau, from the brain (Xie et al., 2013; Louveau et al., 2015; Aspelund et al., 2015; Iliff et al., 2015). Moreover, Iliff and colleagues have provided a series of evidence suggesting that the efficient clearance of interstitial solutes is dependent on the astroglial water channel aquaporin-4 (AQP4), which is localized primarily to perivascular astrocytic end-feet and astrocytic processes of the glial limitans (Iliff et al., 2012; Iliff et al., 2014; Kress et al., 2014; Peng et al., 2016). Loss of perivascular AQP4 polarization is associated with glymphatic pathway impairment in aged mice and AD mouse models Kress et al., 2014; Peng et al., 2016). In the present study, the largest clinical case series to date, they further provided quantitative evidence showing that increasing AQP4 expression is a feature of the aging human brain, and AQP4 mislocalization is related to the glymphatic dysfunction and AD pathology (Zeppenfeld et al., 2016).
Further studies are necessary to clarify whether AQP4 mislocalization in AD is a cause or a consequence of pathology, or merely a parallel event, and how to find specific and nontoxic molecular markers and imaging techniques to detect glymphatic clearance function and abnormal expression of AQP4 in the brain (Iliff et al., 2013; Eide et al., 2015). These potential findings will contribute to establishing AQP4-dependent glymphatic clearance as a novel therapeutic target for the treatment of neurodegenerative diseases associated with accumulation of misfolded protein aggregates.
References:
Ross CA, Poirier MA. Protein aggregation and neurodegenerative disease. Nat Med. 2004 Jul;10 Suppl:S10-7. PubMed.
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, Axel L, Rusinek H, Nicholson C, Zlokovic BV, Frangione B, Blennow K, Ménard J, Zetterberg H, Wisniewski T, de Leon MJ. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015 Aug;11(8):457-70. Epub 2015 Jul 21 PubMed.
Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O'Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M. Sleep drives metabolite clearance from the adult brain. Science. 2013 Oct 18;342(6156):373-7. PubMed.
Louveau A, Smirnov I, Keyes TJ, Eccles JD, Rouhani SJ, Peske JD, Derecki NC, Castle D, Mandell JW, Lee KS, Harris TH, Kipnis J. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015 Jul 16;523(7560):337-41. Epub 2015 Jun 1 PubMed.
Aspelund A, Antila S, Proulx ST, Karlsen TV, Karaman S, Detmar M, Wiig H, Alitalo K. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J Exp Med. 2015 Jun 29;212(7):991-9. Epub 2015 Jun 15 PubMed.
Iliff JJ, Goldman SA, Nedergaard M. Implications of the discovery of brain lymphatic pathways. Lancet Neurol. 2015 Oct;14(10):977-9. PubMed.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012 Aug 15;4(147):147ra111. PubMed.
Kress BT, Iliff JJ, Xia M, Wang M, Wei HS, Zeppenfeld D, Xie L, Kang H, Xu Q, Liew JA, Plog BA, Ding F, Deane R, Nedergaard M. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. 2014 Dec;76(6):845-61. Epub 2014 Sep 26 PubMed.
Peng W, Achariyar TM, Li B, Liao Y, Mestre H, Hitomi E, Regan S, Kasper T, Peng S, Ding F, Benveniste H, Nedergaard M, Deane R. Suppression of glymphatic fluid transport in a mouse model of Alzheimer's disease. Neurobiol Dis. 2016 Sep;93:215-25. Epub 2016 May 24 PubMed.
Zeppenfeld DM, Simon M, Haswell JD, D'Abreo D, Murchison C, Quinn JF, Grafe MR, Woltjer RL, Kaye J, Iliff JJ. Association of Perivascular Localization of Aquaporin-4 With Cognition and Alzheimer Disease in Aging Brains. JAMA Neurol. 2017 Jan 1;74(1):91-99. PubMed.
Iliff JJ, Lee H, Yu M, Feng T, Logan J, Nedergaard M, Benveniste H. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J Clin Invest. 2013 Mar 1;123(3):1299-309. PubMed.
Eide PK, Ringstad G. MRI with intrathecal MRI gadolinium contrast medium administration: a possible method to assess glymphatic function in human brain. Acta Radiol Open. 2015 Nov;4(11):2058460115609635. Epub 2015 Nov 17 PubMed.
Make a Comment
To make a comment you must login or register.