Can Heparin Delay Alzheimer’s Disease?
Quick Links
A drug that has been used for nearly a century to prevent and dissolve blood clots may also delay the onset of Alzheimer’s disease, according to a study in the October 8 Molecular Psychiatry. Heparin may never be prescribed for AD, but the findings reinforce the idea that similar chemicals found naturally in the brain play key roles in the disease.
- In two independent hospital systems, past heparin use was associated with a one-year delay in AD onset.
- It may block ApoE and tau from binding to endogenous heparin-like molecules.
The body’s own heparin-like molecules include heparan sulfate proteoglycans (HSPGs), which serve a wide range of functions in cell membranes and the extracellular matrix. HSPGs bind two proteins implicated in AD: ApoE and tau (Holmes et al., 2013; Rauch et al., 2018). Tau forms the neurofibrillary tangles found in AD brains, while ApoE has been implicated in both tangle and amyloid plaque pathology. ApoE4, the most important genetic determinant of late-onset AD risk, binds more tightly to HSPGs than do other ApoE forms (Arboleda-Velasquez et al., 2019).
For the new study, scientists led by Benjamin Readhead of Arizona State University, Tempe, and Eric Reiman, Banner Alzheimer’s Institute, Phoenix, speculated that heparin might protect people from AD by competing with HSPGs for binding sites on ApoE or tau. To test this, they examined electronic health records of people diagnosed with AD at two large hospital systems in New York City—Mount Sinai Medical Center and Columbia University Medical Center. Even though the two systems had different patient populations, both datasets showed that people who received heparin were diagnosed with AD when they were approximately one year older than people who never received heparin.
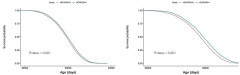
Alzheimer’s Delayed? Survival curves show that in the MSHS (left) and CUMC hospital systems (right), people who had been given heparin (blue line) were diagnosed with AD later than those who were never given heparin (red line). [Courtesy of Readhead et al., 2024.]
“We were interested to see that the apparent protective effect of heparin was actually pretty similar across these different medical contexts,” said Readhead.
Marc Diamond of the University of Texas Southwestern Medical Center in Dallas, who was not involved in the study, echoed the sentiment. “It is important that a small, if statistically significant, effect was observed in two independent cohorts,” he wrote to Alzforum. But he pointed out that people are typically treated with heparin for only a few weeks, and that the amount that crosses into the brain is likely low. For these reasons, he thinks the findings may reflect something other than heparin treatment.
People who receive heparin have conditions that need anticoagulants, such as atrial fibrillation and heart disease, and they often have related comorbidities such as Type 2 diabetes mellitus and cerebrovascular disease. Many of the conditions associated with heparin use are themselves risk factors for AD and are treated with other drugs as well.
But while those comorbidities make it difficult to disentangle the role of heparin, any bias they introduce would be expected to weaken the results, not strengthen them, said Readhead. Indeed, when the scientists statistically controlled for comorbidities, the heparin appeared even more protective, with hazard ratios dropping from 0.89 to 0.69 in the MSSM system and from 0.80 to 0.69 in CUMC.
Readhead hopes that the findings could pave the way for new AD drugs with mechanisms similar to heparin. Moreover, he said, the study highlights the value of analyzing large datasets from electronic health records in a targeted way, with specific hypotheses guided by laboratory research.
“Electronic health records in isolation have all sorts of weaknesses. But the strength of this particular story is that it was very biologically informed by these preceding genetic and then experimental studies,” said Readhead. “If our story leaves me with a lesson, it is the power of combining these different investigational approaches.”—Nala Rogers
Nala Rogers is a freelance writer in Silver Spring, Maryland.
References
Paper Citations
- Holmes BB, DeVos SL, Kfoury N, Li M, Jacks R, Yanamandra K, Ouidja MO, Brodsky FM, Marasa J, Bagchi DP, Kotzbauer PT, Miller TM, Papy-Garcia D, Diamond MI. Heparan sulfate proteoglycans mediate internalization and propagation of specific proteopathic seeds. Proc Natl Acad Sci U S A. 2013 Aug 13;110(33):E3138-47. Epub 2013 Jul 29 PubMed.
- Rauch JN, Chen JJ, Sorum AW, Miller GM, Sharf T, See SK, Hsieh-Wilson LC, Kampmann M, Kosik KS. Tau Internalization is Regulated by 6-O Sulfation on Heparan Sulfate Proteoglycans (HSPGs). Sci Rep. 2018 Apr 23;8(1):6382. PubMed.
- Arboleda-Velasquez JF, Lopera F, O'Hare M, Delgado-Tirado S, Marino C, Chmielewska N, Saez-Torres KL, Amarnani D, Schultz AP, Sperling RA, Leyton-Cifuentes D, Chen K, Baena A, Aguillon D, Rios-Romenets S, Giraldo M, Guzmán-Vélez E, Norton DJ, Pardilla-Delgado E, Artola A, Sanchez JS, Acosta-Uribe J, Lalli M, Kosik KS, Huentelman MJ, Zetterberg H, Blennow K, Reiman RA, Luo J, Chen Y, Thiyyagura P, Su Y, Jun GR, Naymik M, Gai X, Bootwalla M, Ji J, Shen L, Miller JB, Kim LA, Tariot PN, Johnson KA, Reiman EM, Quiroz YT. Resistance to autosomal dominant Alzheimer's disease in an APOE3 Christchurch homozygote: a case report. Nat Med. 2019 Nov;25(11):1680-1683. Epub 2019 Nov 4 PubMed.
Further Reading
Primary Papers
- Readhead B, Klang E, Gisladottir U, Vandromme M, Li L, Quiroz YT, Arboleda-Velasquez JF, Dudley JT, Tatonetti NP, Glicksberg BS, Reiman EM. Heparin treatment is associated with a delayed diagnosis of Alzheimer's dementia in electronic health records from two large United States health systems. Mol Psychiatry. 2024 Oct 8; PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.